You’ve heard the saying: Life is a balancing act.
According to researchers at Augusta University’s Medical College of Georgia, a protein that safeguards against bacterial infections is itself engaged in a precarious balancing act, where the stakes can be life and death.
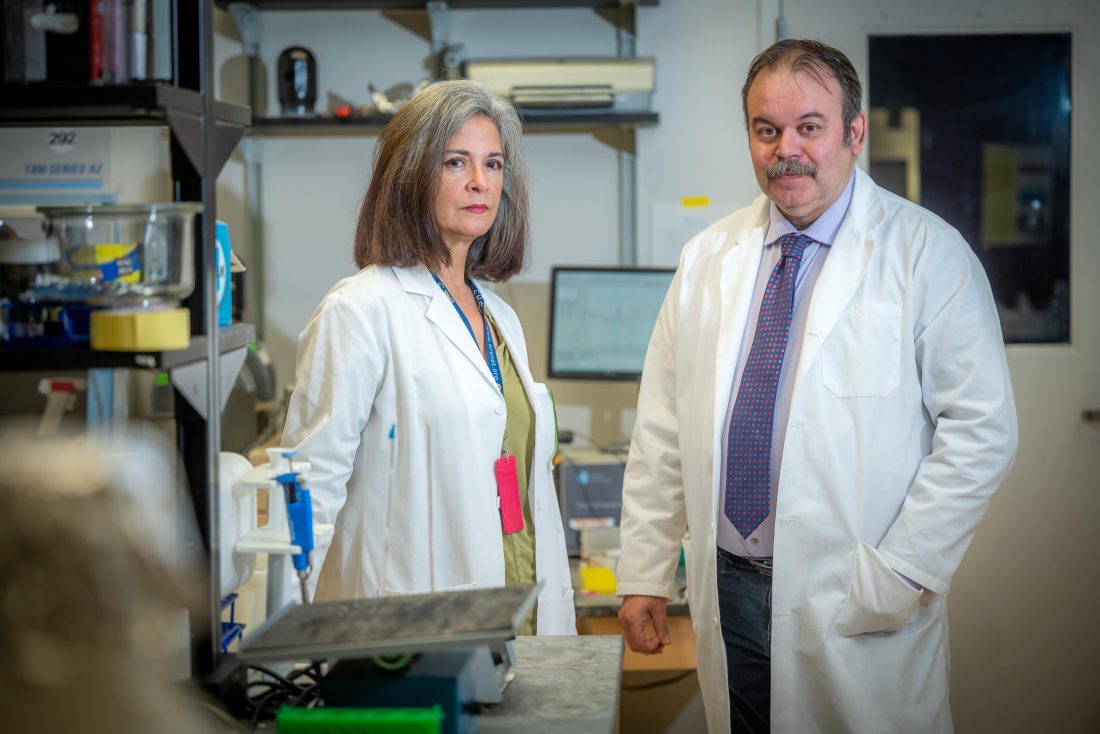
Rudolf Lucas, PhD, a vascular biologist in MCG’s Vascular Biology Center, first author Maritza Romero-Lucas, PhD, and members of the Lucas Lab have dedicated years to developing treatment methods for acute respiratory distress syndrome triggered by pneumococcal pneumonia. ARDS often has underlying risk factors, including bacterial and viral pneumonia, such as in COVID-19.
Those with ARDS experience a buildup of fluid and pus in the air sacs of their lungs, which impairs gas exchange and often leads to serious damage to other organs like the heart, liver and kidneys. This causes a high mortality and significantly reduces the quality of life for those who recover.
The current treatment plan for severe ARDS carries significant risks. While ventilators can provide life-saving airflow, they also bring the risk of bacterial infection and lung damage caused by the high pressure of oxygen flow.
“ARDS has a very poor prognosis, with about 40% mortality,” Lucas said. “Apart from ventilation strategies, there are no proven pharmacological treatments to date, so there is a very high need to develop pharmacotherapies for ARDS.”

That’s where his research team comes in. The Lucas Lab has developed a synthetic peptide, known as the TIP peptide or Solnatide/AP301 in phase 2 clinical trials. This peptide has already been shown to prevent severe pneumonia-associated ARDS and protect kidneys from nephritis. By binding to the alpha subunit of the epithelial sodium channel – which is expressed in both alveolar epithelial and lung capillary cells – the TIP peptide plays a crucial role in activating fluid clearance from the alveoli and in maintaining barrier function, especially when bacteria or bacterial toxins are present.
“I think we are one of the first research groups to show that activation of ENaC in the capillaries can actually help strengthen the barrier function,” Lucas said.
To do so, researchers studied mice that lacked a crucial subunit of the ENaC channel specifically in their endothelium. Without this subunit, newborn mice couldn’t remove lung fluid, leading to fatal ARDS.
“Mice that lacked the crucial alpha subunit of the ENaC channel in the capillaries became much more susceptible to capillary leaks upon pneumococcal infection,” Lucas said. “However, the mechanism of how this worked was a real surprise to us, because we found that the epithelial sodium channel alpha subunit somehow represses oxidative stress in mouse lung capillaries during bacterial pneumonia.”
The oxidative stress in the capillaries seems to be mainly caused by an enzyme called NADPH Oxidase 2, which is normally activated in neutrophils during pneumococcal pneumonia.
“NOX2 is part of the first line of defense, producing reactive oxygen species to kill bacteria,” Lucas explained. “You don’t want to get rid of this enzyme in neutrophils. However, too much NOX2 activity in capillaries directly contributes to barrier dysfunction and increases susceptibility to harmful infections.”
The balancing act of NOX2 is the reason why global inhibitors of the enzyme have not been evaluated in clinical trials, since they would increase susceptibility to infection. But with this discovery, endothelial ENaC could become another therapeutic target, addressing capillary leak-inducing oxidative stress in ARDS without impairing the host’s defense system, since ENaC is not expressed in neutrophils. Moving forward, the Lucas Lab plans to continue investigating NOX2 and other NOX enzymes that could play a role in treating ARDS pharmacologically.
The Lucas Lab’s research has already received positive responses from fellow researchers at the University of Illinois Chicago’s Division of Pulmonary, Critical Care, Sleep and Allergy Department of Medicine. In a recent editorial, Steven Dudek, MD, professor of medicine, wrote the lab’s findings have provided new insights that could “TIP” the scales for patients suffering from ARDS.
Lucas’s study was published in the American Journal of Respiratory Cell and Molecular Biology, in collaboration with co-author Douglas Eaton, PhD, a physiologist from Emory University and a member of the Center for Cystic Fibrosis and Airways Disease Research at Children’s Healthcare of Atlanta and with co-author Michael Matthay, MD, a clinician-scientist at UCSF, who is currently evaluating the efficacy TIP peptide in an isolated human lung model infected with pneumococci. The peptide is currently in a dose-escalating multi-center phase 2b clinical trial in ARDS patients, organized by the company Apeptico, in Vienna, Austria.
Read the study.
Discoveries at Augusta University are changing and improving the lives of people in Georgia and beyond. Your partnership and support are invaluable as we work to expand our impact.
 Augusta University
Augusta University