A synthetic peptide developed by researchers at Augusta University’s Medical College of Georgia could help reduce vascular problems associated with acute respiratory distress syndrome in COVID-19.
In severe cases, COVID-19 is associated with the syndrome, which happens when fluid builds up in the tiny, elastic air sacs in the lungs, keeping them from filling with enough air and keeping oxygen from reaching the bloodstream.
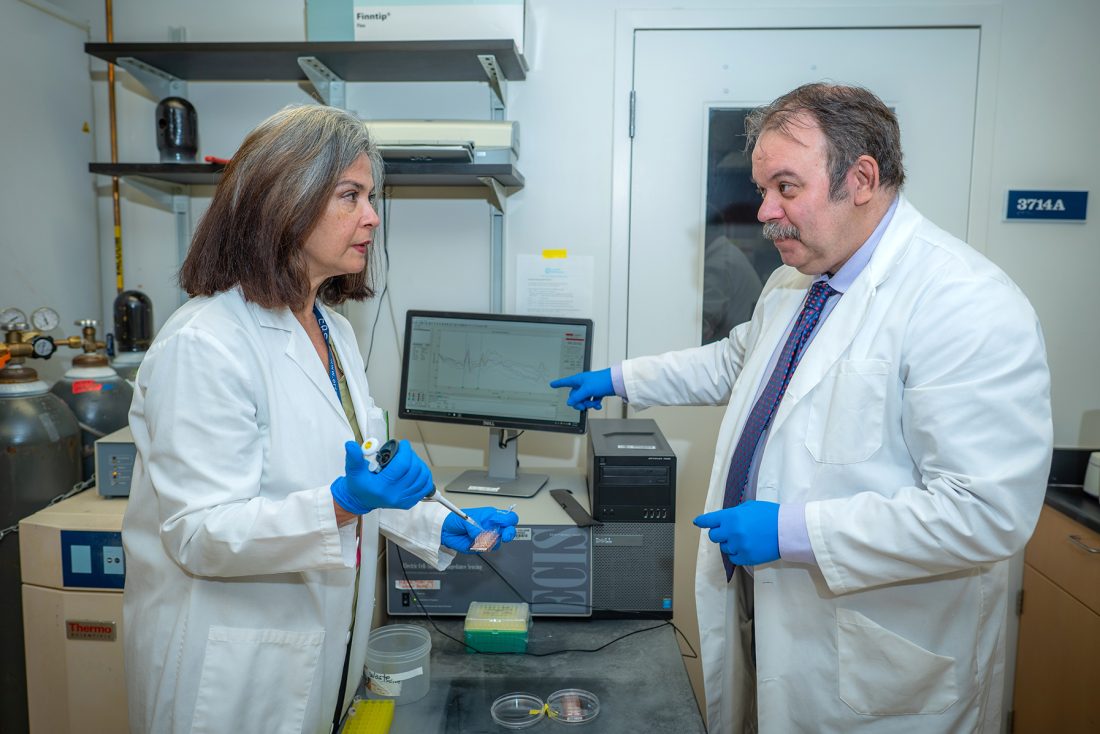
“These are the people who get the sickest from the virus,” said Rudolf Lucas, PhD, vascular biologist in the Vascular Biology Center at the Medical College of Georgia. “It is a pathology with a very bad prognosis. Many of these patients must go on a ventilator and a significant percentage of them succumb.”
Researchers have long known that COVID-ARDS is accompanied by a cytokine storm, when an over-aggressive immune system releases too many of these signaling proteins — which in healthy amounts help stimulate the immune system fight the infection — into the blood stream, which can eventually lead to multi-system organ failure. This cytokine storm can also occur in non-COVID ARDS. Since both severe COVID and non-COVID ARDS have a comparable mortality, Lucas and his team are working to delineate how the former differs from the latter and to identify novel therapeutic avenues.
“In agreement with recent findings by others, we think that what could represent the main difference is that SARS-CoV2-induced ARDS has a much higher vasculopathy, so much higher damage to the vasculature, as compared to non-COVID ARDS,” he explains. “This prompted us, and others, to look for factors specific to SARS-CoV-2 that make the endothelium that lines the blood vessels in the body so dysfunctional.”
When looking at endothelial cells body-wide, researchers have actually reported finding very little virus. What has been found, however, is that levels of the virus’s spike protein, which it uses to bind to receptors throughout the body, are higher in the serum of people with the more severe cases and can be detected even months after clearing most of the infection.
“So, we started looking into whether the receptor binding domain of the spike protein does something to the endothelial cells in the lungs,” Lucas said. “We found that the spike protein — specifically the subunit which contains the receptor binding site — makes endothelial cells dysfunctional.”
Essentially, he explained, the spike protein binds to a receptor — specifically human ACE2, which normally plays a role in protecting cell barriers. The virally induced shedding or downregulation of this receptor can cause the endothelium to start producing more angiotensin 2, eventually leading to more oxidative stress in the endothelium. “That destroys barriers and induces capillary leaks. On top of that this can induce tissue factor production in the endothelium, which can lead to micro-thrombi or tiny clots that are typically found in mass in people who die of COVID-19. Now, we want to know if the spike protein somehow sensitizes the endothelium, leading to dysfunction, and how to counteract that.”
Lucas and his research team have been working for years on a synthetic peptide, called the TIP peptide (known as Solnatide, AP301 in clinical trials) that has already shown promise in protecting kidneys from nephritis and preventing severe pneumonia. It essentially works by binding to a subunit of the epithelial sodium channel, called ENaC alpha, which is mainly expressed in the epithelium, like alveolar epithelium in the lungs, but also in the microvascular endothelium in capillaries. Their peptide has been shown to play an important role in keeping barrier function intact, especially in the presence of bacterial toxins.
Now they’re looking toward these severe cases of COVID-related ARDS, to see if they can use the peptide to prevent the dysfunction induced by the spike protein of the virus, Lucas and his colleagues report in the journal Frontiers in Immunology.
“The reason we are particularly interested in looking at ENaC in this context is that we know the spike protein in SARS-CoV-2 has to be cleaved between its two subunits in order for it to be able to bind to human ACE2,” Lucas said. “That cleavage is done by an enzyme called furin, which cleaves the protein in a sequence of eight amino acids. We already knew that in mammals, only one other protein has an identical cleavage sequence – ENaC alpha, where it is needed to mature the channel. Another mechanism through which the spike protein can impair ENaC is by inducing a protein called protein kinase C (PKC), which also impairs the function of the channel.”
In collaboration with Douglas Eaton, PhD, a physiologist from Emory University and a member of the Center for Cystic Fibrosis and Airways Disease Research at Children’s Healthcare of Atlanta, the team found that the TIP peptide, which binds to the alpha subunit of ENaC, can overcome the inhibitory effect of the spike protein on sodium uptake by the epithelial sodium channel.
“Importantly, the TIP peptide can actually reduce oxidative stress induced by the spike protein and restore human ACE2 surface expression in capillaries,” Lucas said. “We still don’t know exactly how the spike protein induces endothelial dysfunction,” but it does not seem to be extreme enough by itself to cause such vasculopathy.
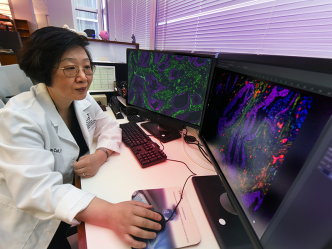
Exploring further, the researchers believed the answer would come in understanding why patients who have both COVID and pneumococcal pneumonia have a mortality rate seven times higher than people with pneumonia alone. Using a similar model, they pretreated transgenic mice expressing human ACE2, generated by Lin Gan, PhD, director of MCG’s Transgenic & Genome Editing Core, with the spike protein and then infected them with Streptococcus pneumoniae. They found a much higher capillary leak as compared to mice which were only infected with pneumococci or mice which were only treated with the spike protein.
“Our findings show that with the combination of SARS-CoV-2 and pneumococcal pneumonia, there is a high increase in tissue factor production and in microthrombi, and all of that was inhibited when the mice were treated with the TIP peptide,” Lucas said. “This confirms our original hypothesis that the spike protein will sensitize the endothelium to become dysfunctional, but this will mainly only happen when there is a second insult.”
While COVID numbers have mostly waned, these findings could have implications in long COVID, which is known to be linked to endothelial dysfunction and increased oxidative stress. The research team has shown that treatment with the TIP peptide, even after spike protein delivery, reduces oxidative stress. “That could imply that regardless of the onset of symptoms, it is still having an effect when it is delivered,” he says. “That is something I would definitely like to look a bit more into.”
The TIP peptide is currently in phase 2 clinical trials in patients with COVID- and non-COVID ARDS in Austria and Germany, organized by the company APEPTICO. It also was approved for compassionate use treatment of severe COVID patients in Italy and Austria.
Read the study.
 Augusta University
Augusta University