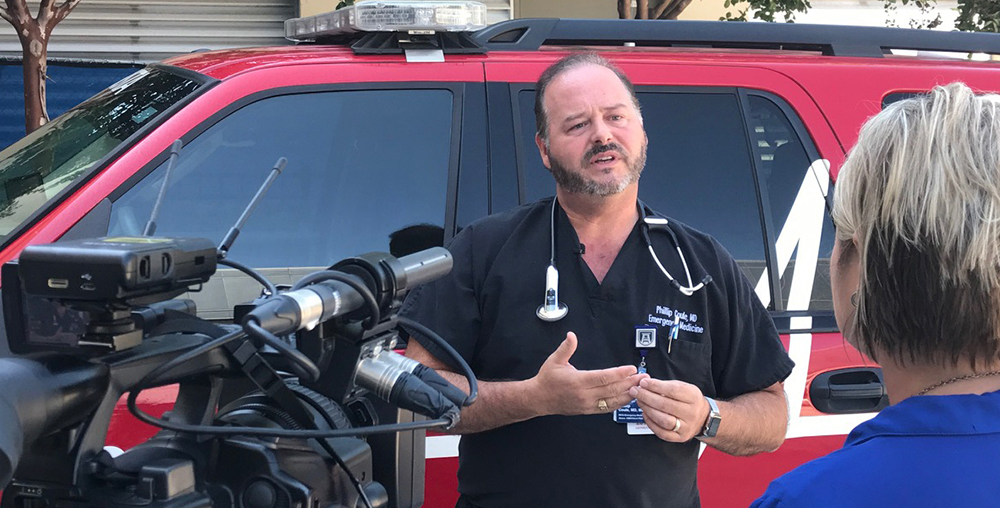
With COVID-19 cases surging locally and across the country, Augusta University Health announced this week that 122 people are currently hospitalized with COVID-19 and the medical center’s ICU is at capacity, according to Dr. Phillip Coule, vice president and chief medical officer for AU Health.
“We don’t have any ICU beds left,” Coule said, adding the upcoming Labor Day weekend will only increase the number of COVID-19 cases in the area. “Unfortunately, we’re predicting that it’s going to get worse. Please get vaccinated if you haven’t already.”
With only 51.9% of the people in this country fully vaccinated, COVID-19 hospitalizations have been on the rise in the United States since early July. The number of COVID-19 hospitalizations across the country has nearly tripled in the past month.
In Georgia, only 43% of the population is estimated to be fully vaccinated, according to the Georgia Department of Public Health.
Locally, the numbers are even more discouraging, with only 32% of Richmond County residents and 37% of Columbia County residents being fully vaccinated.
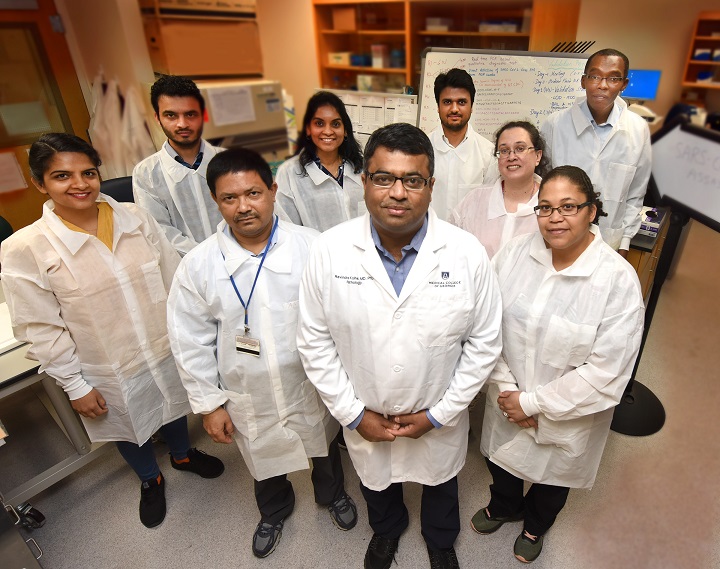
The unvaccinated are fueling the spread of COVID-19 and the highly infectious Delta variant throughout the country, said Dr. Ravindra Kolhe, director of the Georgia Esoteric and Molecular (GEM) Laboratory at Augusta University and vice chair for translational research in the Department of Pathology at the Medical College of Georgia.
“If you’re following the numbers of the COVID hospitalizations, there is such a day and night difference between unvaccinated and vaccinated individuals,” Kolhe said. “There is no comparison.”
Of the 122 COVID-19 patients currently hospitalized at AU Health, 116 of those patients are unvaccinated.
As of Aug. 30, there are 52 patients with COVID-19 in the ICU and only two of those people have been vaccinated. Of the 37 patients currently on ventilators, only two of those patients have been vaccinated, according to AU Health.
“You can’t get better facts than that,” Kolhe said. “The truth is, a vaccinated individual might get exposed to COVID and you might be symptomatic, but the rate of hospitalization and requiring oxygen as a treatment or even ventilation is less than 1%.”
Get vaccinated
Despite the medical community’s efforts to encourage more people to get vaccinated, the United States hit an unfortunate milestone last week. More than 100,000 people are currently hospitalized with COVID-19 in this country, the first time the U.S. has surpassed that mark since January, according to data from the U.S. Department of Health and Human Services.
In Georgia, there are currently more than 55 hospitalizations per 100,000 people, according to HHS data.
Even more worrisome is the fact COVID-19 hospitalization rates among children and adults under 50 are the highest they have ever been, according to the Centers for Disease Control and Prevention.
The latest report from the American Academy of Pediatrics and the Children’s Hospital Association found COVID-19 cases among children have quadrupled in the past month from about 38,000 cases a week near the end of July to more than 180,000 cases in children by mid-August.
With the rapid increase of the highly infectious Delta variant, as well as the even more concerning Delta-plus variant, Kolhe strongly encouraged people to get the COVID-19 vaccine, not only to protect themselves, but also to protect children under 12 who currently cannot get vaccinated.
“There is a significant population which is not eligible for vaccination, especially children and the immunocompromised,” Kolhe said. “So, if you’re not vaccinated, not only are you acting as a safe haven for these viruses to evolve, but you are also putting our vulnerable populations — especially our children — at risk because they can’t get vaccinated at this moment.
“I think it’s our duty as a community to get vaccinated if you’re eligible in order to help protect those who can’t get vaccinated.”
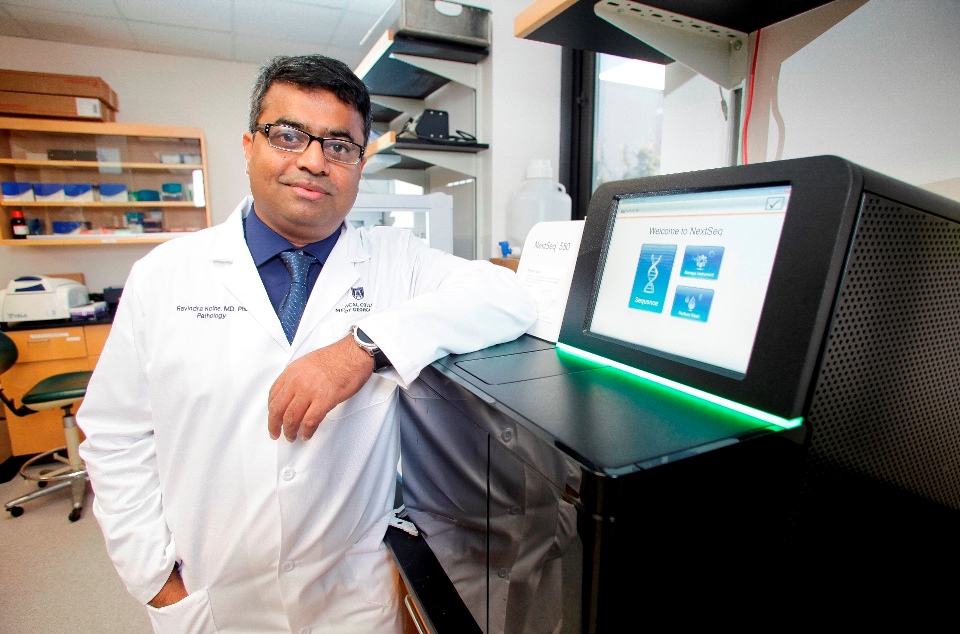
Kolhe was pleased that the U.S. Food and Drug Administration fully approved the Pfizer vaccine last week for those 16 and older.
“There was this hesitancy among some individuals saying, ‘Oh, this vaccine is not FDA approved,’” Kolhe said. “Well, now it’s an FDA-approved vaccine, so that shouldn’t be a concern anymore. The amount of work behind this vaccine is phenomenal. It is one of the safest and highly studied vaccines we’ve ever had.”
The next step is to get children ages 5 to 11 to become eligible to receive the COVID-19 vaccine, he said.
“I really hope by Thanksgiving we should have the FDA approval for children ages 5 to 11,” Kolhe said. “My wife is a pediatrician and our kids will be first in line to get their vaccine.”
Studying COVID-19
Data from the GEM lab at Augusta University had the first confirmed sequences of Delta and Delta-plus in the Augusta area. From about 400 samples taken by the GEM lab during the summer months, 142 were the Delta strain and more than 30 were the Delta-plus variant, Kolhe said.
A previous sequencing report of samples from the GEM lab that ran through the end of May found neither the Delta strain or the Delta-plus variant.
“As the evolution of this virus has continued, variants started becoming more prominent and aggressive, and, at the moment, the Delta variant is the prominent one across the globe,” Kolhe said. “Now, we have new mutations added in the Delta and some people call it the Delta-plus variant.”
The best tool to stop these variants from continuing to spread and mutate is for the country to achieve herd immunity by vaccinating at least 80% of the population, Kolhe said.
“The pockets of the communities where the rate of vaccination is really low, those pockets act as a harbor for this virus to multiply rapidly and evolve,” he said. “Then those communities spread it across to the other areas of the country. Vaccination is going to be so critical in curtailing this virus. We need 80% of the people to get vaccinated.”
Just last year, Kolhe recruited 500 local frontline workers for a year-long study to find out what percentage tested positive for the COVID-19 virus and whether the antibodies they produce protect them from reinfection.
Kolhe’s study is part of a National Institute of Allergy and Infectious Diseases-funded project totaling $1.9 million called the SARS2 SeroPrevalence And Respiratory Tract Assessment, or Project Sparta.
“Every month, we look at the health care workers, as well as community members, on their current infectious status by testing saliva and then their antibody status by blood,” he said. “The idea is to see how long the natural immunity stays, because one of the misconceptions in the community is, ‘If I was infected with COVID last year, then I don’t need the vaccine because that infection itself will help me prevent the next infection.’
“But people have to understand that even if you were infected by COVID last year, the natural antibodies are produced against the original virus, and those antibodies are not only going down in quantity, but they are relatively ineffective against the newer variants.”
It is similar to the need for a person to get a flu shot every year, Kolhe said.
“If you look at our experience with flu, we don’t take the exact same flu shot each year,” Kolhe said. “Or, even if you had the flu last year, you still take a flu vaccine because we know that this year’s flu is going to be different than last year’s flu because it’s a different strain.”
The only difference is, COVID-19 and the variants are much more contagious than the flu, he said.
“The coronavirus is a lot more aggressive,” Kolhe said. “This virus is going to create more symptoms, it’s going to create more rapid symptoms and it’s going to create faster damage to a patient’s system.”
Long-term effects of COVID
One of the major concerns Kolhe has about COVID-19 is the possible long-term effects of the virus.
“We know a lot of patients experience some shortness of breath and then they get treated. But at this moment, we really don’t know the long-term effects,” he said. “We also know that it definitely affects the neurological system because some people lose their sense of smell and taste, which is very fundamental. But we don’t know what other neurological things COVID is going to affect, especially in children.”
Children are vulnerable because their bodies are still developing, so the long-term impact on them is still an unknown, Kolhe said.
“We really don’t know the impact on children because the original virus, for some reason, was ineffective in children,” he said. “Last year, kids were not getting infected. There were very few cases across the world. But with the new variants, kids are getting sick, they’re symptomatic and we really don’t know how long those effects will stay in them.”

The bottom line is, the best way to protect yourself, your family and your community is to get vaccinated, Kolhe said.
“I think when people think about COVID, they think of it last year,” Kolhe said. “But what we saw last year was something which was very natural in the sense that it was the original virus. A lot of people got sick. A lot of people died because we didn’t know how to treat it. Now, we know how to treat it.”
But this year is a completely different story. The COVID of 2020 is not the COVID of 2021, Kolhe said.
“The virus has become so aggressive that the disease itself has changed, to the extent that I won’t even call this the original virus because it’s totally changed,” he said. “It’s transmitted really fast. A lot of people are getting symptomatic. A lot of people are getting sick. And a lot of people will die.
“The one thing we definitely know is, if you’re vaccinated, there’s a much less chance that you’ll get sick. If you’re vaccinated, there’s less than 1% chance that you will be on a ventilator or that you will die from this virus. So, I encourage everyone to get vaccinated. It could save your life.”
 Augusta University
Augusta University