As the COVID-19 pandemic came to Augusta, it created numerous challenges for health care leaders and staff in the areas of intensive care unit (ICU) bed capacity and respiratory therapy services, amongst many others.
To address these challenges, Augusta University Health teams across Patient Care Services have utilized their collective critical thinking skills and expertise to address these challenges through the conversion of medical/surgical floor beds to ICU beds and intermediate care beds, as well as dramatically increasing respiratory therapy services on all units.
The expansion of some services and the shrinking of others required the re-allocation of staff and the acquisition of new knowledge and skills to safely function in the new and changed environments.
AU Health’s Surge Plan was first put into use on March 18 on 5 West (5W), the designated COVID-19 med/surg unit, when they admitted the first COVID-positive patient.
Assistant Nurse Manager (ANM) Kathryn Mathis acknowledges the anxiety the staff felt.
“I have to admit, we were at first really scared and mentally not ready, but when the challenge came, so did the teamwork,” she said.
Mathis immediately began partnering with Venita Davis, 4W/5W ANM, and Jeremy Graham, nurse manager 4W/5W, and their charge nurses to coordinate the requisition, distribution and training for required personal protective equipment (PPE) needed to protect the patients and staff.
“Venita and I spent a lot of time just helping staff feel safe and making sure they had the resources they needed to protect themselves and provide safe care,” she said.
Mathis held team huddles every morning at 7:05 a.m. where she reviewed a sheet of CDC guidelines and told the staff, “I know you are scared, but this is what we will do to protect ourselves.”
The 5W staff partnered with the hospitalists and Information Technology to develop the needed electronic order sets for required PPE and other treatments. Mathis also describes sharing the recommended PPE information with ancillary staff who provide services on their unit to include Radiology and Environmental Services (EVS).
As she frequently reminds everyone on 5W, “You’re safe, we are going to make it through this and provide good care to our patients. We’re protected because we’re knowledgeable. Don’t be afraid. We got this.”
The 5W transition also required the acquisition of new knowledge and skills in respiratory care and new competencies in the use of nebulizers and other respiratory treatments by nursing staff.
Deborah Bradshaw, a charge nurse in 5W, said teamwork was required to get the job done.
“We had to work closely with Respiratory Therapy (RT) because we had to provide respiratory treatments to the COVID patients because the therapists were needed for the more acutely ill patients,” Bradshaw said. “All we had to do was call RT if we felt uncomfortable or needed help and they were right there.”
To accomplish this job under such difficult circumstances, she said, “We all stick together; we’re all in this together.”
Dipti Donald, 5W clinical outcomes manager, commented on the collaboration between 5W and Nursing Education, Central Supply and EVS.
“It took all of us working together to get the job done well,” Donald said, also mentioning the impact of the support her team felt from leadership. “We had lots of support from the top, which really helped the morale of the staff and we appreciated that.”
As the Medical Intensive Care Unit (MICU) reached its COVID-19 patient peak during the week of April 9, other components of the Surge Plan were initiated, with 7 North (7N) modifying its traditional scope of service to become the intermediate unit for non-COVID 6S patients, while 6S began its transition to a non-COVID ICU.
This change required the 7N leadership and staff to partner with Nursing Education and Research Department, MICU leadership, and 6 South leadership to develop a plan for the staff to gain the necessary knowledge and skills to safely provide care in their new capacities.
According to Christa Butler, NM, 4S and 7N, the unit transition and the rapid acquisition of new skills was a time of “overwhelming excitement mixed with nervous anticipation.”
“We are very used to change, but not at the COVID-19 pace,” Butler said. “We ‘rallied the troops’ on our team and developed and shared the education strategy. (The 7N team) has fully embraced this opportunity to expand their skill sets and are honored to be a part of the solution to this much larger problem facing our health system and the world at large.”
LaDonna Walker, clinical outcomes manager, echoed that working together was key. “This effort required phenomenal teamwork. I called on all my peers and everyone came to the table.”
Paul Smith, NM, 6 North and his staff, along with Nursing Education staff and Pharmacy, assisted the 7N staff in gaining new knowledge and skills in cardiac monitoring, intravenous drug infusions and respiratory treatments. Learning new skills rapidly can be quite challenging, especially to RNs newer in practice.
Morgan Connell, RN, one of the newest on the unit, said, “The more experienced nurses make it very easy to go to them. I feel very supported, even though this is a big challenge.”
These patients presented with major respiratory problems and during the early days of the surge, it was primarily emergent and acute care. The respiratory therapists for the ICU and ED teams had to be reorganized and staffed up to meet those urgent needs.
According to Jennifer Anderson, director of Respiratory Services, the Surge Plan required the RT leadership team to come together and take a look at all the therapists across inpatient and outpatient services.
“The focus was adult intensive care but we had RTs in Pediatrics, Pulmonary Function Lab, Bronchoscopy Intervention Team and the Sleep Disorders Lab,” Anderson said. “We had to come up with a rapid plan to cross train, review and check off staff who had been out of adult critical care for a while but also educate on ventilators we rented to provide for the volumes we were experiencing.”
Marianne Ferrell, RRT, a therapist on the Bronchoscopy Intervention team based in the PFT Lab, quickly returned to the department she started in as a new graduate to cover 12-hour shifts. “It was easy for me to return to ICU care as I had been in the department for many years before I went to my new assignment.”
Shelliece Williams, RRT based in Adult RT, added, “Everyone came together and worked hard to make sure we were able to do what needed to be done.”
Raymond McHatton, RRT, said, “There were additional precautions we had to learn to use while caring for these patients, which was new to all of us.”
After a short time, it was evident that RT would need the help of the nursing staff on the floors to take over those procedures so the ED and ICUs could be covered. Nursing education teamed up with RT to get education to the nursing team in the entire hospital.
What a great model for teamwork and collaboration, said Chief Nursing Officer for Augusta University Health, Laura Brower.
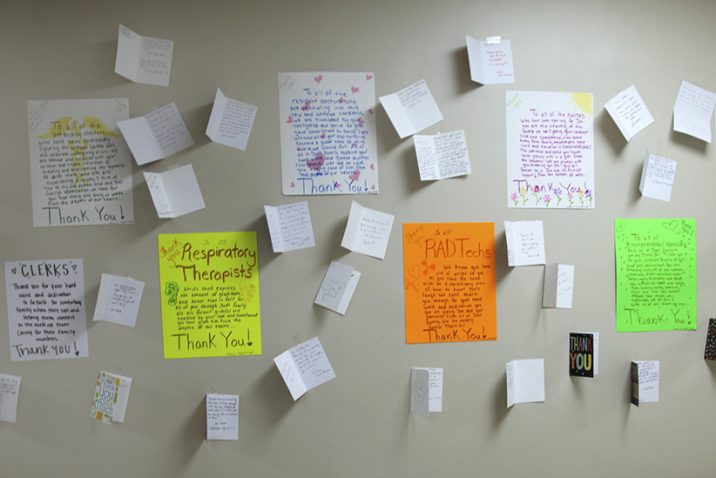
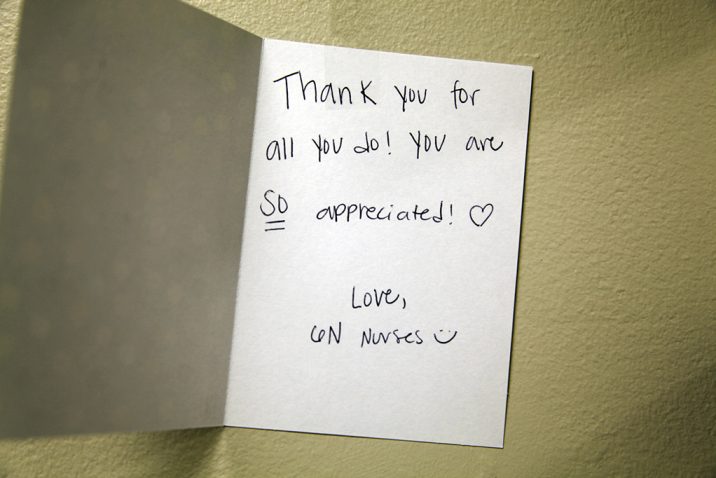
“The teamwork and collaboration represented here are just are just a few examples of those occurring within Patient Care Services at AU Health,” she said. “Thank you all for your commitment to the team, your patients, and each other. You are our HEROES!”
 Augusta University
Augusta University