AUGUSTA, Ga. – Immune cells that are ready to take action against invaders like bacteria have been found in women’s breast milk, researchers say.
They say the presence of this SWAT team of immune cells called innate lymphoid cells, or ILCs, in human breast milk is more evidence of the benefits of breastfeeding.
Short term, the ILCs in breast milk may help protect newborns from infection, and longer term help babies develop their own protective immune system, they report in JAMA Pediatrics.
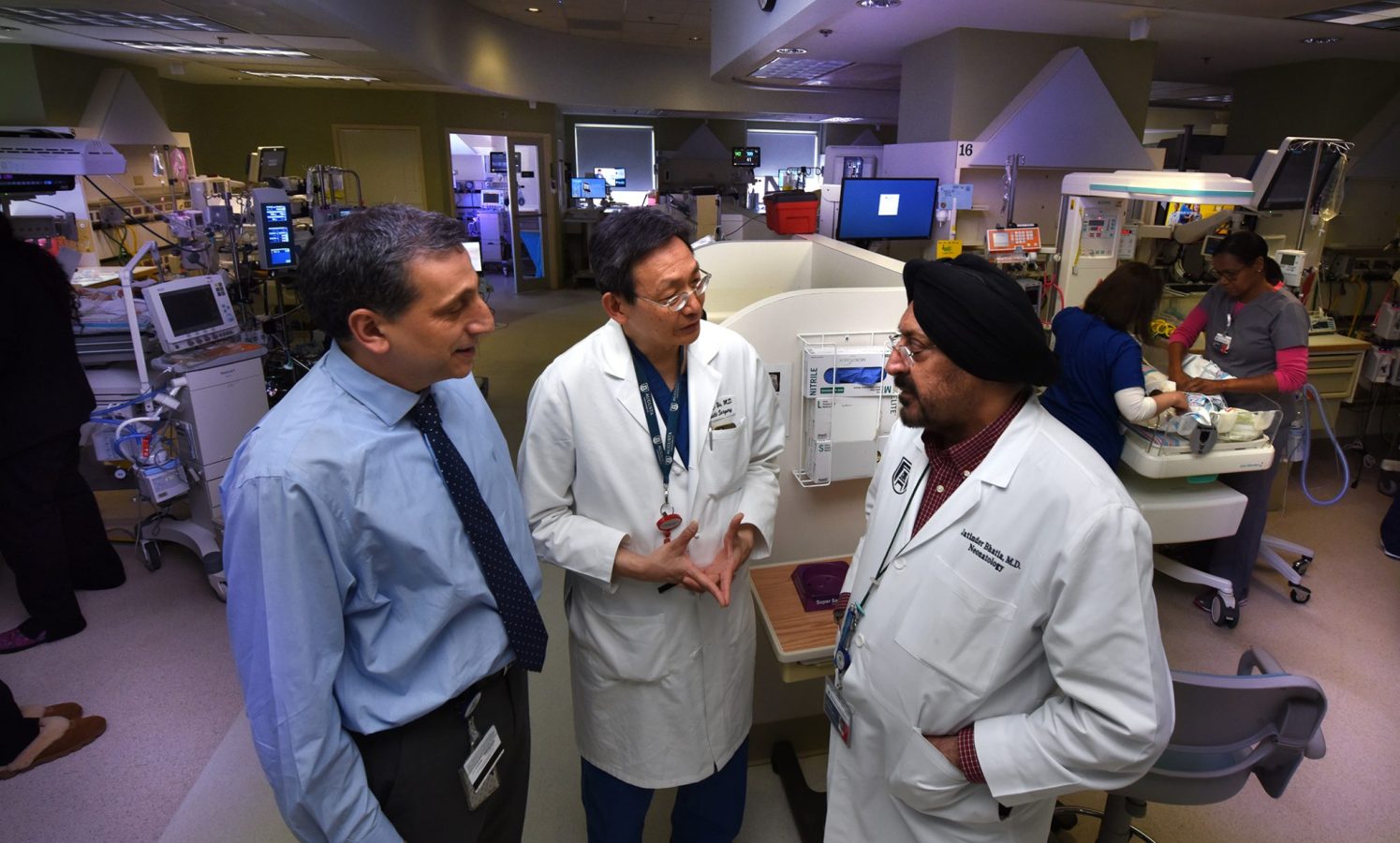
“We were looking for the source which can provide immune protection to the baby while it develops its own immune system,” says Dr. Jack Yu, chief of pediatric plastic surgery at the Medical College of Georgia at Augusta University.
“We think these cells help provide frontline immune protection for the baby,” says Dr. Jatinder Bhatia, chief of the Section of Neonatology and vice chair of clinical research in the MCG Department of Pediatrics.
“These cells are upstream of the immune response … we know they can initiate and advance an immune response,” adds Dr. Babak Baban, immunologist in the Department of Oral Biology in the Dental College of Georgia at AU and in the MCG Department of Surgery.
They found all three known classes of ILCs present in fresh human mother’s milk – type 1 is the most prevalent – and parallel mouse studies show that the cells not only are transferred to baby by nursing but that they survive in the baby’s gut for at least several days.
Now they want to learn more about what happens to the ILCs once they get to baby’s gut and how/if they help tailor the baby’s microbiome, which aids digestion and infection protection and typically is very similar to mom’s, particularly with breast feeding.
“The moment you are born, you start to build a microbiome,” Yu says. Their preliminary findings, including the parallel mouse studies, indicate ILCs are a player in the construction. ILC3s definitely have a role, Baban says of this ILC type that helps form the protective mucosal layer for the gut and respond to the microbiome when it does develop.
The researchers think the ILCs in the breast milk may also be a way to protect mom from getting an infection from the suckling baby. The cells may even be part of the dynamic that enables the content of breast milk to change to help the baby get over that infection.
“There is a feedback loop,” says Yu. It’s known that some immune cells like leucocytes, another white blood cell that fights infection, increase in the milk in response to an infection in the baby. The researchers still don’t know if the newly found ILCs do the same but suspect that ILCs are part of the cue to the mom that something is amiss with her baby.
ILCs of all types are known to locate in tissues throughout the baby’s body during development, where they appear stationary and inactive, waiting for a developed immune system to communicate with, says Baban, the study’s corresponding author. “Until then, these cells are like a central command in each tissue with no soldiers,” he says adding that the ILCs transmitted in breast milk may help provide those soldiers.
Scientists have only been studying ILCs for about a decade, and they have been found to be important in inflammation, immunity and tissue homeostasis.
It’s known that mother’s milk contains millions of cells, including a lot of immune cell types. But this appears to be the first time ILCs have been reported to be among the cell types, Yu says.
In fact, the largest immune cell population in breast milk is macrophages, which ILCs are known to direct. Macrophages, which literally means ‘big eaters,” are the largest of the white blood cells and much-better studied than ILCs. They are known for their ability to envelop unwanted items like bacteria, viruses and dead body tissue, and can also help incite or calm inflammation.
ILCs, although always ready for a fight, don’t do the attacking themselves rather send cytokines – proteins important in cell signaling – to tell the macrophages what to do, Baban says.
Bhatia, who has chaired the American Academy of Pediatrics Committee on Nutrition, is an advocate for breastfeeding, including for the premature babies in his neonatal ICU at Children’s Hospital of Georgia. When mother’s milk is not available, the NICU team uses donor breast milk. Bhatia notes that formulas today more closely mimic mother’s milk, including containing nutrients like the essential omega 3 fatty acid, DHA, associated with brain development, and lactoferrin, a protein that aids iron transport and has anti-infective properties.
The researchers note that while the cells can survive the acidic environment of the stomach, ILCs and many other helpful cells don’t survive refrigeration. For the newly published study, the researchers did extensive cell analysis on fresh milk from four lactating women.
The baby does has some other frontline protection provided by immunoglobulin G, the most common antibody in our circulation and the only one that can journey through the placenta to the baby, Baban says.
 Augusta University
Augusta University