Electronic medication monitoring caps may help physicians put together the puzzle of why children taking a medicine that promises to curb sickle cell disease are showing mixed, confusing results.
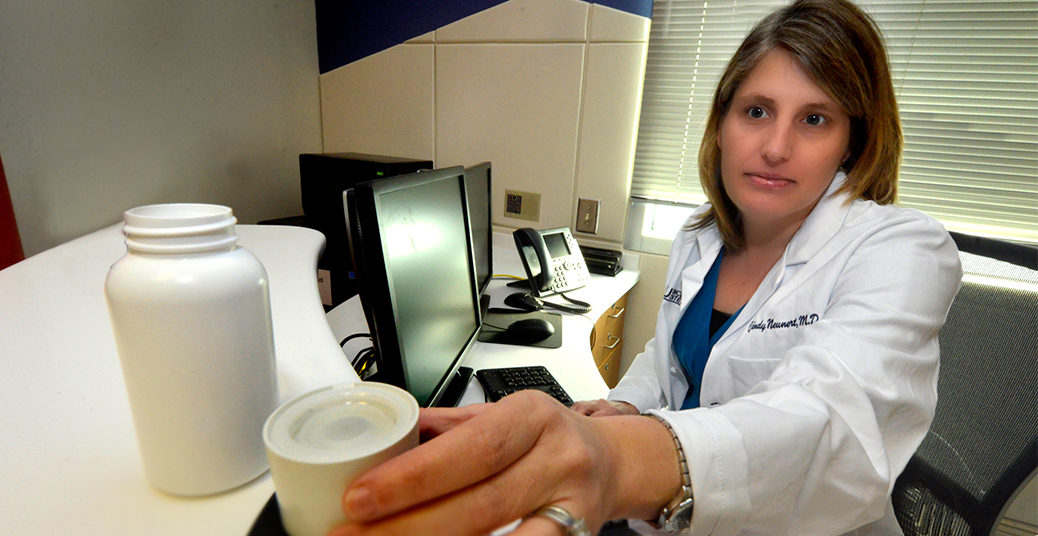
Clinical studies indicate that children who take hydroxyurea, the only Food and Drug Administration approved drug for their condition, will have fewer pain crises, hospitalizations, and other related problems, said Dr. Cindy Neunert, pediatric hematologist/oncologist at the Medical College of Georgia at Georgia Regents University.
Still, physicians such as Neunert are finding that laboratory results and how well patients are actually doing on the medication often conflict. Patients taking the medication may not have positive laboratory results – such as higher blood levels of fetal hemoglobin, which can’t sickle – yet they are feeling and doing better. Others have great lab reports but don’t seem to be doing better. Even some who say they aren’t taking the drug regularly can paint a mixed picture.
Neunert is Principal Investigator on a new study, funded by the National Heart, Lung, and Blood Institute, seeking to put the pieces together by establishing a method to accurately monitor medication use, examining medical and social barriers to its use, and exploring genetic differences between patients who do and don’t respond.
“It feels like we don’t have the whole picture. We have kids who clearly tell us they are taking it, and we don’t see the right blood changes,” Neunert said. “We have kids on very small doses that have great effects. We also see kids who clearly have a clinical benefit without having much of a lab benefit. There is all this variability in numbers and response so I am very interested in looking at what role adherence does play. What are our labs really telling us and how can we best monitor use?”
Her pilot study will follow a group of 50 children, age 2 to 18, on the drug who regularly come to Children’s Hospital of Georgia in Augusta for care, as well as those seen by MCG faculty in the south Georgia city of Valdosta, about 4 1/2 hours away.
Hydroxyurea, which has been on the market since the 1960s as a chemotherapy drug, was approved by the FDA for adults with sickle cell disease in 1998. Sickle Cell Centers such as MCG’s have been using it in children with severe symptoms for about a half-dozen years based on its success in adults when used as prescribed. More recently, a large series of clinical trials showed that the majority of children with sickle cell disease can benefit. The final, phase 3, placebo controlled clinical trial of the drug in 193 children beginning at age 9 to 18 months indicated decreased rates of initial and recurrent pain episodes, including severe pain in the bones of the hands and/or feet, as well as hospitalizations.
The BABY HUG findings were published in the journal Blood in November 2012 and the drug should be considered for all children age 9 months and older, Neunert said. However, it remains unclear who is not taking the drug versus who is simply not responding, and why they aren’t taking it, if that’s an issue.
The medication monitoring cap will provide a downloadable record of the date and time a medicine bottle is opened, and researchers will compare that approach of measuring adherence to more common ones such as pill counts and prescription refill rates. They’ll also compare adherence data to laboratory changes expected with taking the medication, such as bigger red blood cells and fewer inflammatory cells.
Researchers also will be keeping up with how many transfusions the young patients need, how much pain they have, and how many hospitalizations. In the laboratory of Dr. Betty S. Pace, Tedesco Distinguished Chair in Pediatric Hematology/Oncology and Interim Chief of the Section of Pediatric Hematology/Oncology, they will also examine the children’s blood for any genetic differences in apparent drug responders versus non-responders.
They’ll also explore if/why some children may not be getting the drug. Increased doctor visits that accompany taking the daily pill definitely increase the burden of care for families. Particularly with children who were not symptomatic before, health care providers may need to do a better job understanding families’ reservations about starting the drug as well as explaining its benefits, Neunert said.
Monthly doctor visits and more frequent laboratory monitoring, as opposed to quarterly or as-needed, may be a particular burden for families living in more rural areas. While MCG faculty, including Neunert, travel to cities such as Valdosta every other month to see patients, taking hydroxyurea still means a lot more trips to Augusta for families to see a sickle cell expert. Neunert notes that in a separate initiative, the sickle cell physicians are pursuing the use of telecommunications technology to reduce families’ travel burden without compromising care.
Ideally, examining all these clinical pieces will clarify the issues and identify targeted solutions. “How does the clinical picture match with the adherence picture and match with the laboratory picture to maybe describe some patterns of response and nonresponse with hydroxyurea use?” Neunert said.
The new study is part of an $8.8 million NHLBI grant exploring new therapies for sickle cell anemia under the direction of Sickle Cell Center Director, Dr. Abdullah Kutlar. Neunert is a participant in the Hemoglobinopathy Translational Research Skills Training Core, funded by the grant and led by Pace to inspire and prepare the next generation of sickle cell researchers.
Neunert’s study is among the first to use the new Children’s Research Unit in the Children’s Hospital of Georgia that is enabling more clinical studies with children. According the NHLBI, about 70 percent of drugs given to children have not been tested in children.
 Augusta University
Augusta University