Earlier this year, a team of researchers in the Department of Psychiatry and Health Behavior at the Medical College of Georgia at Augusta University was awarded a $2.5 million National Institutes of Health-sponsored grant seeking to address a two-sided condition that impacts millions of people across the globe.
Now, they’re seven months into the five-year Assessing Improvements in Mood and Sleep, or AIMS, Trial, that could end up saving countless lives.
The relationship between insomnia and depression
For the past several decades, studies on the correlation between insomnia and depression have been published in scientific journals, with an increase in this research over the last 15 or so years.
These studies and surveys show a strong bidirectional comorbid relationship between sleep problems and depression, meaning they can be caused by each other, and they often occur at the same time. In fact, an article in Current Psychiatry Reports estimates that people with insomnia are five times more likely to have anxiety or depression symptoms than people without it.
And it’s not just people of a certain demographic being affected. Research shows people of all ages from around the globe are affected.
To target this correlation, the MCG team worked with two other institutions, the University of Pittsburgh and the University of California, Los Angeles, to develop the AIMS Trial.
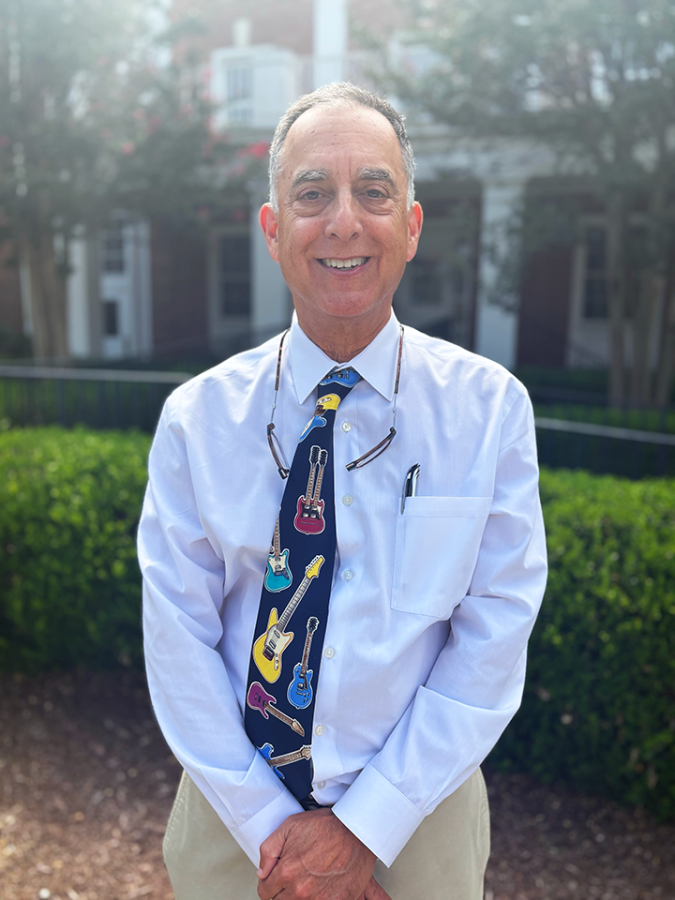
“Ultimately, the hope is to find other avenues to reduce the risk for depression and depression symptoms,” said William Vaughn McCall, MD, professor emeritus in the Department of Psychiatry and Health Behavior and the principal investigator of the study.
Past research
In 2019, McCall and his research team published a study testing the effectiveness of zolpidem, a prescription sleep aid commonly known by its brand name, Ambien, in treating outpatients who had insomnia and depression symptoms.
The results of the experiment showed reduced symptoms of insomnia, depression and suicidal ideation in the test group.
“After that paper came out, there were a variety of groups around the country that wanted to go in a different direction and see if the same results can be achieved without pills, which is what we’re doing in this trial,” McCall said.
Solving the problem without the pills
The AIMS Trial will be using forms of psychotherapy, in which the patients speak to trained mental health professionals to identify and change certain patterns or behaviors.
“The present study is riffing off of all this prior literature about an association between sleep problems and depression symptoms. Our prior work showed that drug therapy of insomnia may reduce depression symptoms, but we’re now moving it to a different modality in the form of psychotherapy intended to address sleep problems in a focused group of older patients,” McCall said.
He went on to explain that there are already types of psychotherapies that are used to target sleep problems.
“One form of psychotherapy is called Cognitive Behavior Therapy for Insomnia, or CBTI. But there are broader applications of sleep psychotherapies that go beyond what CBTI is interested in, and we are comparing these different approaches,” McCall said.
Savannah Makowski, the site therapist for the study, will be using two types of talk therapies that are focused on sleep and depression to treat the patients’ symptoms.
“It’s a very structured eight-week protocol, and we work through very specific skills with their sleep,” Makowski said.
“To expand, the psychotherapies used in this study are skills-based interventions that are individualized to the participants’ presenting concerns,” continued Jessica Britt-Thomas, PhD, an associate professor in the Family and Community Medicine and Psychiatry and Health Behavior departments and the co-investigator of the study.
Specific information regarding trial methodology is confidential to protect the integrity of the study.

Implementing the AIMS Trial
After years of putting the pieces in place, the team found out they were receiving the grant back in April.
“We were ecstatic because you put these things in so far in advance, and then we got a late notification that the grant had been approved,” said Laryssa McCloud, PhD, research manager in the Department of Psychiatry and Health Behavior. “We were very, very happy.”
Along with AU, UCLA and the University of Pittsburgh are also test sites, with Pitt serving as the parent site. So far, the AU team has enrolled 14 participants and has other interested parties in the pipeline.
The three sites are all currently recruiting patients ages 55 or older who are diagnosed with depression and are on antidepressant medications but still have active symptoms. While some participants might prefer to come to the MCG psychiatry department in person, it’s also possible to complete all aspects of the trial remotely.
“It’s mostly with referrals to our psychiatry department. We will consider people who are referred to the department and see if they might be eligible for the study,” McCloud said. “We also have groups that we are working with to screen people who may be a part of their group, and they’ll help us determine whether or not they may be someone who’s interested and eligible for the study. We also have flyers around the hospital.”
“We’re really open to receiving information from any sources about possible participants. I wouldn’t turn down a phone call from anybody who thought they or their loved one might benefit from being in this study,” McCall added.
People selected for the study will complete their eight weeks, then follow up for five months afterward.
“Tess Dzurny and I are study assessors, so we recruit and assess potential participants for the study and do their screening,” said Joely Fields, a research assistant in MCG’s Department of Psychiatry and Health Behavior. “They have assessments that are done throughout the study to see if they’re eligible, and then we see how they’re doing as they progress.”
The goal is for each site to have 140 participants in the study over the course of the five years.
“The total budget period for the study is five years, but patients are entering and exiting across the five years,” McCall said. “Each patient is being studied for about seven months, but it takes us five years to accrue as many people as we need to complete the goals.
“We are hopeful that this study, as we develop it further, will allow a relationship with Wellstar to allow us to treat patients across the state inside this research protocol,” he continued. “That would be exciting and potentially exemplary for other studies that could come down the pipe outside of psychiatry in other departments.”
 Augusta University
Augusta University




