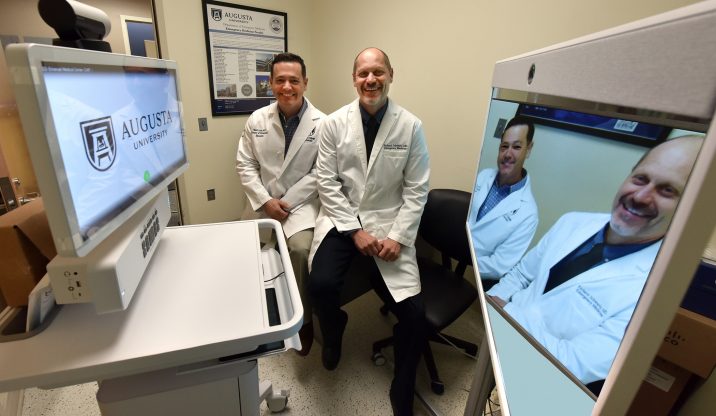
Emergency medicine physicians at the Medical College of Georgia at Augusta University are helping rural hospitals better treat patients by establishing tele-emergency departments.
With a nearly $369,000 telemedicine grant from the United States Department of Agriculture, physicians at the state’s only public medical school have equipped five rural Georgia emergency rooms with a mobile cart that allows them to remotely consult with emergency physicians in Augusta at MCG and AU Health. The carts, which have teleconferencing equipment and software, portable point of care ultrasound machines and airway devices, allow physicians at these hospitals to perform basic diagnostic tests and procedures, guided by MCG physicians, and keep more patients in their emergency rooms instead of immediately transferring them to larger hospitals with emergency medicine trained physicians.
“The entire program is built on a true partnership model,” says Dr. Richard Schwartz, chair of the Department of Emergency Medicine at MCG and principal investigator on the grant. “These hospitals tell us what they need and we design the system with them in mind. We want to enable them to provide a higher level of emergency care than they’ve been able to offer up to this point.”
“There’s never really been, from an emergency standpoint, a telehealth system that has worked well for the state,” adds Dr. Matt Lyon, vice chairman for academic programs and research in the MCG Department of Emergency Medicine and a co-investigator on the grant. “Previous systems have failed because of two main barriers – equipment and cost. The grant enables us to provide the equipment at no cost to these hospitals.”
The carts are in emergency rooms at Wills Memorial Hospital in Washington; Emanuel Medical Center in Swainsboro; Washington County Regional Medical Center in Sandersville; Miller County Hospital in Colquitt; and Crisp Regional Hospital in Cordele. The tele-EDs will be staffed 24 hours a day by MCG emergency medicine physicians.
Emergency rooms in rural hospitals are often staffed by non-emergency medicine trained physicians because hospitals can’t afford emergency medicine specialists, Lyon explains. Enabling those physicians to consult with emergency medicine trained physicians at AU Health can help patients get better care and help rural hospitals remain open.
“One of the problems we face, particularly in rural Georgia, is that hospitals close because they’re not financially viable,” he says. “They don’t have enough volume because people don’t go there and those that do go don’t stay. We see transfers (to AU Health) for very minor things, like a lumbar puncture (used to diagnose serious infections like meningitis), for example. We could save a third of transfers for radiology – like evaluating for pregnancy location – just by having ultrasound there. Our goal is to help them keep people in their hospitals. We can do that with telemedicine.”
The partnership has other benefits as well. If patients do need to be transferred to a larger hospital or trauma center like AU Health, the consulting physicians can make that easier. “It’s obvious that if a patient has something like a brain bleed, they need to be transferred,” Lyon, a 1999 MCG graduate, says. “It can be hard to get into a big hospital, but we can expedite the transfer process for them.”
Rural hospitals also have what are called “swing beds,” meaning they can change the bed’s status to suit the care needs of patients – a bed dedicated to surgery recovery could be changed to a bed dedicated to inpatient rehab, for example. At AU Health and other tertiary and quaternary care hospitals, under rules of the Centers for Medicare and Medicaid Services, bed status cannot be changed. “So, if a person breaks their hip and has surgery to repair it, we can do the surgery here and send them to a hospital near their home for inpatient rehab and ongoing care,” Lyon says. “Or if someone needs long-term acute care, we can send them there. That helps us and these rural hospitals because they have the volume they need and patients aren’t getting readmitted here, which we’re penalized for by CMS.”
Schwartz and Lyon are also working to expand the program to the state prison system. “We get a lot of transfers from prisons, which costs the state a lot of money in ambulance fees,” Lyon says. “We’re working with officials at Johnson State Prison in Wrightsville to see if we can expand this program and provide more care in the prison.”
This program is just one example of how the MCG Department of Emergency Medicine is working to improve care throughout rural Georgia. Physicians at MCG travel throughout the state teaching rural emergency room providers basic procedural courses in ultrasound and basic and advanced life support. The department, in collaboration with the Georgia College of Emergency Physicians, also hosts an annual Rural Emergency Practice Conference to train health care providers from across rural Georgia in the latest and best practices in emergency medicine.
 Augusta University
Augusta University