Margaret Trevathan wasn’t sure what to expect when she was floated to the Medical Intensive Care Unit (MICU) to care for patients who are critically ill with COVID-19, and she was apprehensive.
Her anxiety stemmed from the near constant updating of information surrounding the virus and her lack of experience caring for COVID-19 patients — she is a registered nurse in Neurology Intensive Care and usually cares for patients with conditions such as stroke, Parkinson’s or other disorders of the nervous system. Compounding her anxiety was the risk of bringing the virus home to her dad, who is in his 70s.
“I was concerned there wouldn’t be enough equipment or supplies to protect myself,” she said.
Her concern mirrors that of many other nurses at Augusta University Health, as roles are shifted throughout the hospital to accommodate an influx of COVID-19 patients while still caring for non-COVID-19 patients.
As positive COVID-19 patients were expected to be admitted to the hospital, Patient Care Services administration carefully and quickly developed a hospital-wide surge plan in conjunction with nursing and physician leadership while designing its COVID-19 staffing plan. These preparations, coupled with the plan made by MICU staff and leadership, ensured appropriate resources were in place at the time the first COVID-19 patient arrived.
Trevathan said when she first arrived in MICU, she was overwhelmed by the fear of the unknown. But she found herself relieved and impressed as she partnered with the experienced MICU nurses and learned their processes for providing care to the COVID-19 patients.
“I was concerned things would be disorganized or chaotic and wondered if the staff would have time to help me get acclimated to all the precautions,” said Trevathan. However, she found they had made substantial preparations, such as arranging IV pumps and monitors outside patient rooms and providing a detailed poster instructing on how to don and doff personal protective equipment (PPE) both inside and outside of patient rooms.
“It gave me something to focus on. It gave me reassurance that I was doing everything I needed to do (to stay safe),” she said.

Trevathan’s apprehensions were also shared by MICU nurses.
“When we were identified as the first COVID-19 ICU, everyone was anxious about our ability to care for our patients and keep ourselves safe,” said Hannah Richardson, MICU charge nurse.
But the MICU staff immediately rose to the challenge, reaching out to colleagues across the country to determine best practices for preparing themselves and their equipment for COVID-19 patients.
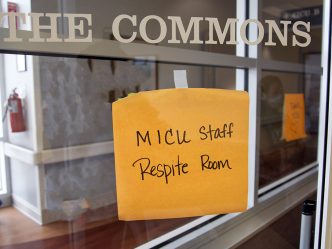
“Our MICU staff quickly transitioned the unit to not only receive COVID-19 patients, but also receive supplemental staff from other areas in our hospital as part of the COVID-19 staffing plan” said Sandra Clay, MICU nurse manager.
In response to COVID-19, Patient Care Services administration developed its plan to account for the need to orient and redeploy staff to support an increase in staffing requirements on both COVID-19 and non-COVID-19 overflow units.
“It’s important to understand that our COVID-19 staffing plan is more than just about taking care of COVID-19 patients on the designated COVID-19 units; it’s about redeploying and optimizing our resources to take care of all our patients while also taking care of and supporting our staff,” said Carol Brody, director of nursing excellence. “There’s a lot of reallocation going on in the hospital and clinics, so not all of the staff that are being redeployed from their home unit are going to take care of COVID-19 patients. They’re being reallocated so that we have adequate staff throughout the hospital wherever the needs are.”
Abbie Gurley, an RN in the Neonatal ICU, was assigned to work in the MICU as part of COVID-19 staffing plan. She admitted that the idea of supporting the care for adults was intimidating because she’s trained to care for children. But she said assisting in the MICU was a positive experience.
“The MICU is a terrific team. They are so knowledgeable and keep up with their research. They made it a really memorable experience for me. I was able to help all of the nurses and look forward to the opportunity to return,” she said.
 Augusta University
Augusta University