AUGUSTA, Ga. – An enzyme that converts testosterone to estrogen appears to have significant impact in a healthy and injured brain, scientists report.
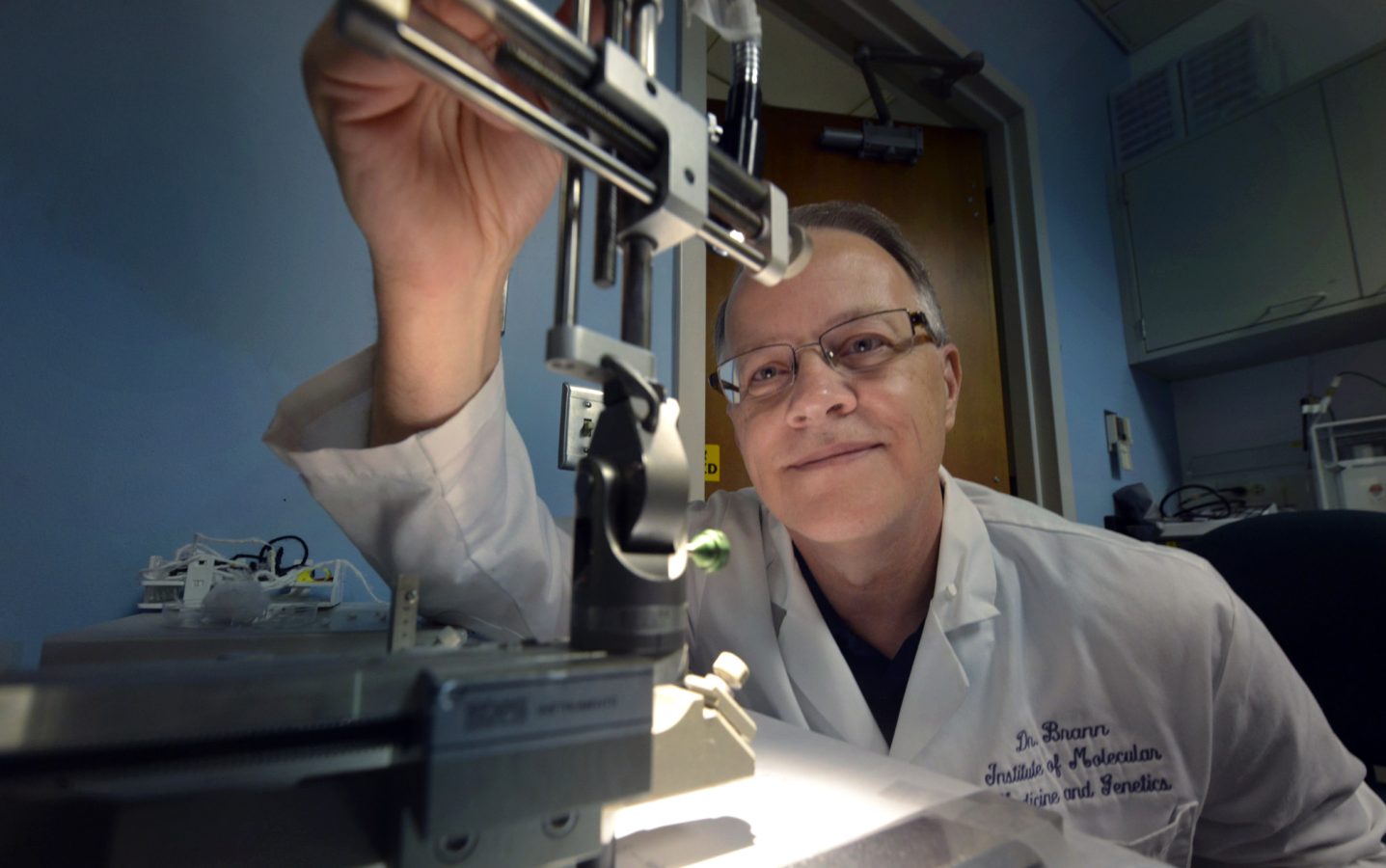
There’s mounting evidence that in the healthy brain, aromatase and the estrogen it enables neurons to produce, helps keep our brains and us nimble. Now scientists are learning that with injury, aromatase and estrogen expression seem to shift to cells in the brain called astrocytes, aiding their support and nurturing of now-stressed neurons, said Dr. Darrell Brann, Regents’ Professor and Vice Chairman of the Department of Neuroscience and Regenerative Medicine at the Medical College of Georgia at Georgia Regents University.
Several studies, including those in Brann’s lab, have shown this primary shift in aromatase/estrogen expression from neurons to astrocytes following injury. In Brann’s case, the studies have been in the hippocampus, a center of learning, memory, and emotions. When he used a drug to reduce astrocyte’s aromatase expression in that region, increased inflammation and brain damage resulted.
A new $1.8 million grant from the National Institutes of Health will enable him to further elucidate the role of aromatase and estrogen in injury and in health and, ideally, point toward therapies that can augment the brain’s apparent effort to heal.
The studies are enabled by the development of several laboratory mice, one with aromatase removed from neurons, another with it missing in astrocytes, and a third with aromatase missing in both brain cell types. The mice were developed by Brann’s lab in collaboration with Dr. Ratna K. Vadlamudi, Professor of Obstetrics and Gynecology at the University of Texas Health Sciences Center.
“We will be able to tell the cell-specific function of estrogen,” Brann said. “We want to know what happens when they don’t have it. We’ll study the plasticity, the connectivity of neurons in these knockouts, and we’ll study their cognitive function using behavioral tests.” They’ll also see what happens to inflammation and recovery when aromatase expression can’t increase as it probably should following injury.
Brann is not surprised that usually supportive astrocytes would take it up a notch following injury and thinks estrogen is critical to the expanded role. “In a non-injury situation, we see it mostly in the neurons, so it much have some functions such as plasticity and connectivity normally,” he said. Following injury, when astrocytes start making aromatase then estrogen, the emphasis appears to shift to protection and recovery.
He notes that as with every built-in protective mechanism, astrocyte support is not foolproof; sometimes natural recovery mechanisms get overwhelmed by the extent of injury. However, Brann hopes that, in addition to better understanding what estrogen does in the brain normally and following injury, the new studies will point toward new therapies that augment the apparent natural recovery effort.
Aromatase is highly expressed by neurons in a healthy hippocampus. After a traumatic injury or stroke, the high expression appears to shift to astrocytes, a type of glial cell, found in abundance in the central nervous system that normally provide support and cushion for neurons. Astrocytes are known to become more active following brain injury, releasing more supportive, healing factors that many scientists believe also help reduce inflammation and increase their protection of neurons. However, if astrocytes remain activated too long they can also cause problems, including gliosis, which is essentially a scar-like wad of glial cells in the space living neurons previously occupied. “You have to tightly regulate all these factors being released,” Brann said.
Even in culture, neurons will connect and communicate, but when scientists add an aromatase inhibitor to the mix, connectivity is interrupted. Some of the first in vivo studies in zebra finches showed that aromatase levels increased following a brain injury, which also supports a protective role for the protein. More brain damage results when aromatase inhibitors are given. “There seemed to be more inflammation,” Brann said.
Part of what he wants to learn about how estrogen aids brain connectivity and plasticity, is exploring whether it regulates brain-derived neurotrophic factor, which is known to have a role in both.
Brann also plans to pursue the role of aromatase and estrogen in neurodegenerative disease, such as Alzheimer’s, where there is some early evidence that missing aromatase increases plaque development.
Naturally high estrogen levels in premenopausal women have long been considered protective of stroke as well as heart attacks and other maladies.
###
 Augusta University
Augusta University