AUGUSTA, Ga. – When trauma spills the contents of our cell powerhouses, it can evoke a potentially deadly immune response much like a severe bacterial infection.
A drug that cleaves escaped proteins called N-formyl peptides appears to reduce resulting dangerous leakage from blood vessels and improve survival, report researchers at the Medical College of Georgia at Augusta University.
The research drug deformylase, or something similar, may one day be a novel treatment for patients with systemic inflammatory response syndrome, or SIRS, a body-wide inflammatory reaction to trauma or infection, as well as sepsis, a systemic infection when the cause of the infection, like a bacteria, is known.
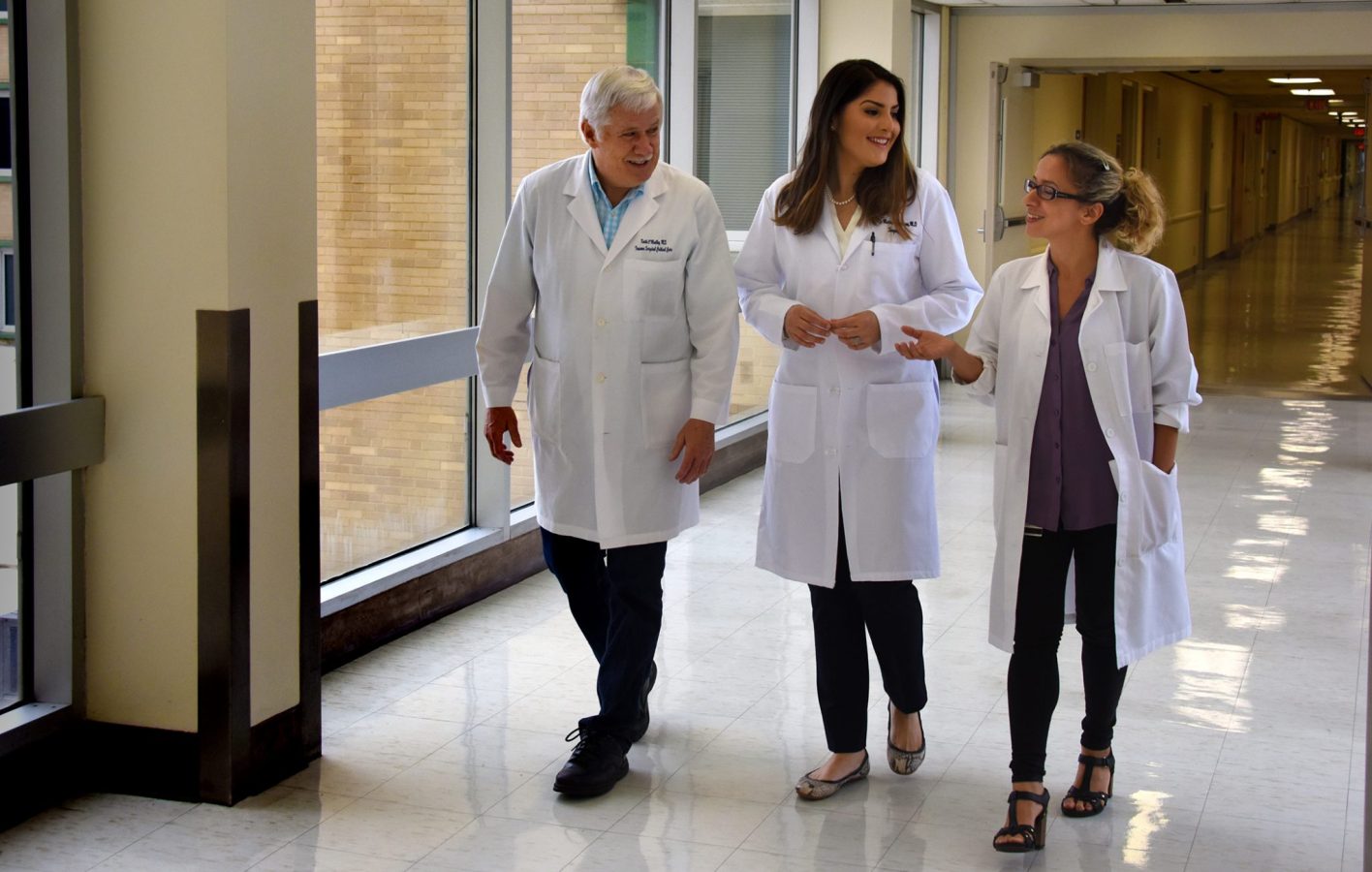
“We are hoping our work will improve the care of trauma and other critically ill patients,” says Dr. Patricia Martinez Quinones, general surgery resident at MCG and AU Health.
Martinez Quinones is presenting the work in both animal models and human cells during the Oral Presentations by Young Investigators session on the final day of the Shock Society’s 41st Annual Conference June 9-12 in Scottsdale, Arizona.
“Once mitochondria (cell powerhouses) are damaged, they just break apart and their contents spill into the circulation,” says Martinez Quinones.
Michondria use N-formyl peptides to make energy for our cells but significant volumes outside the powerhouse can quickly become a detriment. Deformylase appears to neutralize them by removing their formyl group – a combination of carbon and oxygen atoms with hydrogen.
This formyl group is part of every bacterial protein as well as all 13 proteins made by mitochondria, says Dr. Camilla Ferreira Wenceslau, research scientist in the MCG Department of Physiology and senior author of the ongoing studies.
“That is what triggers the immune system to trigger an inflammatory cascade,” says Dr. Keith O’Malley, interim chief of MCG’s Division of Trauma/Surgical Critical Care and a co-investigator on the ongoing studies.
In fact, the mitochondria themselves can similarly neuter the proteins and those benign versions are normally the only ones it releases, until there is an injury.
“The entire hypothesis behind this – and it’s called the danger theory – is that our mitochondria used to be bacteria so when their contents are released our body treats them like an infection,” Martinez Quinones says.
The results can be pretty much the same as if external bacteria entered our bodies: rapid heart rate, fever, precipitous drop in blood pressure and swelling.
“Trauma releases fragments of mitochondria that still carry the signature from bacteria,” says Wenceslau.
If outside bacteria are the source of the immune reaction, an antibiotic should quell the resulting cascade of damage, O’Malley notes. But despite the similarities, there are no known antibiotics that target spilled mitochondrial contents, Martinez Quinones adds.
Deformylase, or something like it, on the other hand may one day be useful at both infective sepsis from an invader and this “sterile” sepsis from our own mitochondria, she notes.
In the lab of MCG physiology chair Dr. R. Clinton Webb, the investigators have looked at a mouse model of sepsis. They’ve also incubated human endothelial cells that line the aorta with N-formyl-rich plasma taken from patients with severe trauma.
Deformylase improved sepsis survival in their animal model by 28 percent and prevented separation of the tightly knit human endothelial cells that keep blood vessel content contained.
“What we saw is that there was a marked improvement in the vascular function of the animals that were treated with deformylase meaning that the vessels that were leaky and couldn’t contract now could,” Martinez Quinones says. “Also, once we treated the plasma with deformylase, the endothelial cell disruption went away.”
Their findings to date have them theorizing that circulating levels of mitochondrial DNA and N-formyl peptides might one day be good biomarkers that could change both how patients are monitored and treated, Martinez Quinones says.
Five years ago, the researchers showed that N-formyl peptides have a powerful relaxant effect in rat arteries that carry blood from the aorta to the gastrointestinal tract. They surmised that when high levels are present, following trauma and other disease, it exacerbates dilation of the arteries and low blood pressure as well as inflammation.
In a study, published last year in the Journal of Trauma and Acute Care Surgery, they looked daily at levels of mitochondrial DNA and N-formyl peptides in the fluid of patients with an open abdominal wound following a significant injury. They found that a routine flushing of the area significantly reduced levels of N-formyl peptides. They hypothesized then and are now studying whether more frequent flushing can help those patients keep levels low and reduce their risk of SIRS and sepsis.
Current studies have them looking in the peritoneal fluid, blood and urine at levels of these peptides in patients who are getting the standard irrigation of the area every 48 hours versus every 24 hours, Martinez Quinones says. If they find more frequent flushes control the levels, that could be sufficient for patients like these with access.
However O’Malley notes that many trauma patients as well as patients with other tissue-damaging disease like cancer and pneumonia do not have ready access at the injury site.
The current version of deformylase they are using has an extremely short half-life so their many pursuits include a more stable version that could be used clinically for those patients, Martinez Quinones says.
The single layer of endothelial cells lining blood vessel walls, which ensure that contents stay inside, are a major target when the body perceives a major infection like sepsis. Patients can experience what’s termed vascular collapse, so they lose tone and the body gets less blood. The typically tight juncture of endothelial cells get lost so blood vessels become leaky and fluid seeps into nearby tissue prompting dangerous swelling in organs like the kidneys and brain. In a sort of vicious cycle, this worsening scenario prompts production of things like oxidative stress and nitric oxide, which exacerbate problems like inflammation and low blood pressure.
“When you are in shock, you only retain about a third of the fluid in your bloodstream,” O’Malley says. “The rest of it seeps out.” Blood pressure drops dramatically, and patients can end up in shock and nonresponsive, he says.
While the results are clear – and potentially deadly – the mechanism which results in the vascular dysfunction is not clear, the researchers say.
Sepsis is the second leading cause of death in non-coronary care ICUs in the United States, with a mortality rate of up to 45 percent, according to the Society of Critical Care Medicine.
During the Shock conference, Martinez Quinones also is being honored with the Diversity Enhancement Award, which encourages pursuit of careers in biomedical sciences. Martinez Quinones, a graduate of the University of Puerto Rico School of Medicine, recently enrolled as a PhD student in the physiology program at MCG and The Graduate School at AU.
The research is supported by the National Institutes of Health.
 Augusta University
Augusta University