Telehealth has seen a surge in popularity in recent years, thanks in part to the COVID-19 pandemic; however, a recent study published by in Mayo Clinic Proceedings: Digital Health shows there is a large divide between rural and underserved communities and other parts of the country in access to high-speed internet, making it difficult for people living in those areas to take advantage of online health services.
It’s a problem that is exacerbated by the fact that rural and underserved communities also tend to have less access to regular health care and are at higher risk for many diseases and other health conditions.
The study featured Neil J. MacKinnon, PhD, executive vice president for academic affairs and provost of Augusta University, as the senior author alongside first author Diego Cuadros, PhD, researcher and epidemiologist with the University of Cincinnati. The team also included researchers from the University of Washington, the University of Hawaii and Hoakkaido University in Japan.
READ MORE: Visiting scholars bring international experience to Augusta University
“Telehealth has an awful lot of merit, but the challenge is that telehealth assumes a person has access to high-speed internet. If someone doesn’t have that access, it can make it difficult for patients and doctors alike. This study shows that because of the digital desert concept, the technology divide really could have health consequences by contributing to a greater health divide in the country,” MacKinnon said.
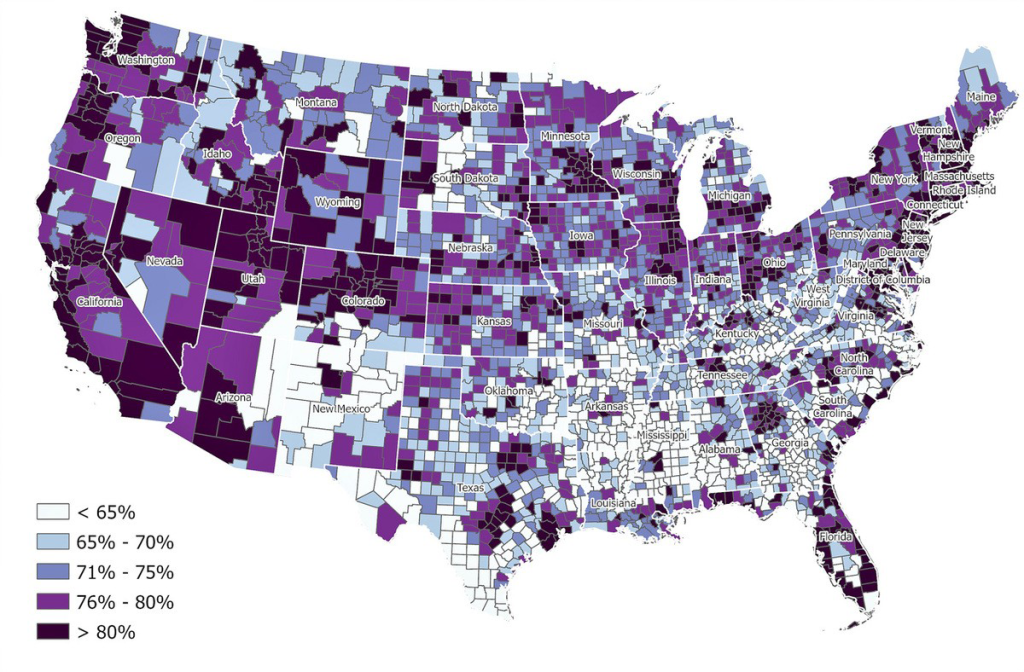
The team conducted a county-level data visualization and spatial analyses of over 3,100 counties across the contiguous United States to assess the geospatial association between digital deserts — areas without broadband internet — and three measures of health care and social vulnerability. The study highlighted disparities in access to digital technology that could widen the gap in access to health care.
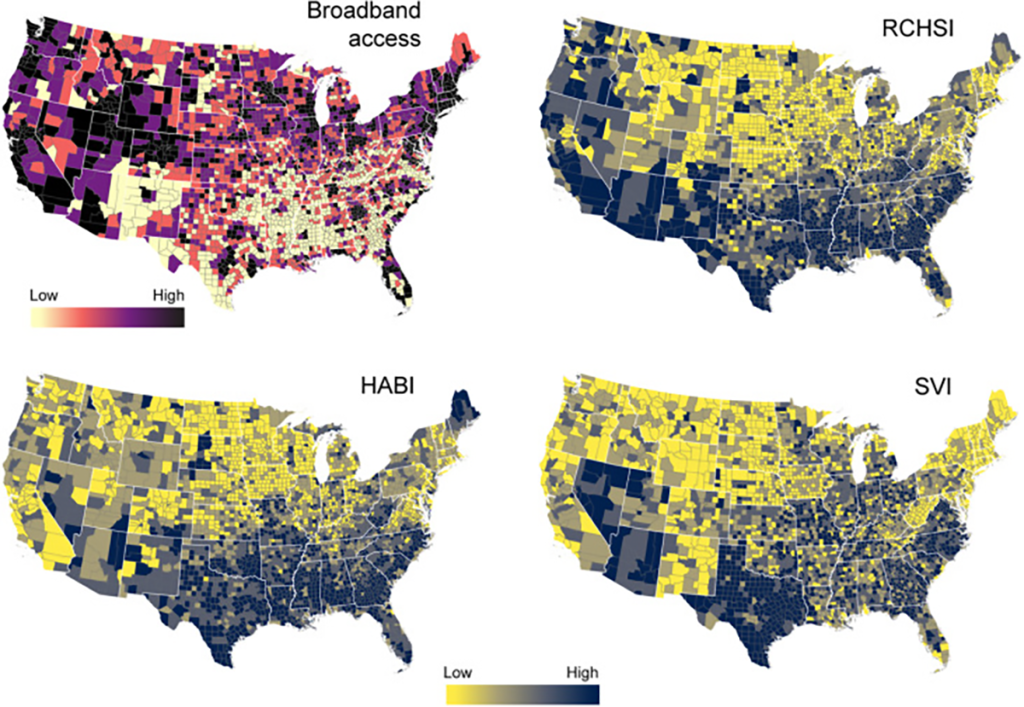
“We identified parts of the country that have poor high speed internet access, and attempted to determine if there is a relationship between that and three different indices, two related to the type of health care available and one based on social vulnerability,” said MacKinnon.
“We found there is a strong relationship between parts of the country in digital deserts that also have limited access to regular health care and are at high risk for many health issues. Through this analysis, we were able to divide the country into four clusters. Cluster 1 is worrisome because that’s where people don’t have high-speed internet access and they are more at risk in health factors with less access to regular health care, and that is where we find most of Georgia, other than Atlanta and a few other select counties.”
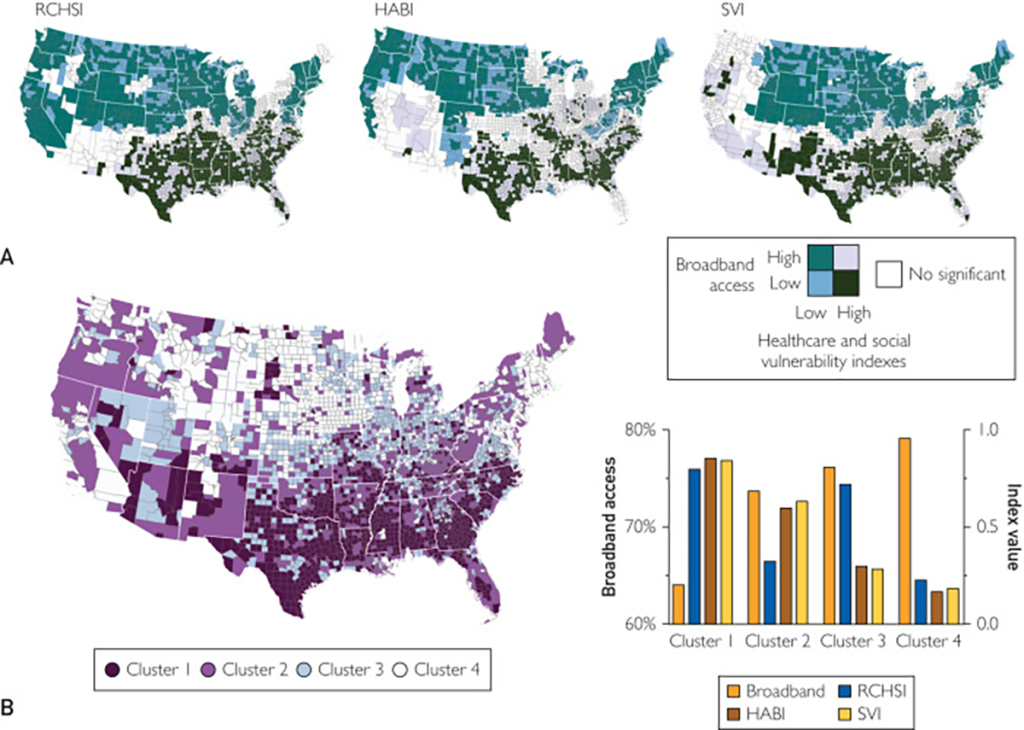
There is no surprise that much of the southern rural United States, stretching from Texas up through North Carolina, is in Cluster 1. This is where access to high-speed broadband internet access is lowest, but resource-constrained health systems are most concentrated. There are also numerous health care accessibility barriers and high social vulnerability.
“The point is telehealth is not going to be useful to everybody. It will be extremely useful to people who already have good access to health care, but it’s not going to be very useful to those who don’t,” Cuadros said. “The digital divide is already here. But in the future, we’ll be even more reliant on these technologies, so that divide is only going to get bigger. The pandemic was a tipping point for us. These technologies are here to stay. That’s how we’ll experience a lot of aspects of our life, from education to relationships to health care.”
While the United States is a global telecommunications leader, it does not even crack a list of the top 20 nations in terms of per capita wireless coverage, according to a 2023 Statista survey. Part of that is due to the size in square miles of the US.
The Biden administration announced in March it will invest $73 million in outreach grants to provide affordable high-speed internet to more Americans. The program is designed to address a growing gap in access to health care created during the COVID-19 pandemic when providers began offering more health care services over the web.
Augusta University announced earlier this year that $1 million in federal funding was secured by U.S. Rep. Buddy Carter to help support the recently established Medical College of Georgia Center for Telehealth.
The funding will support Augusta University’s mission to improve health care access and outcomes for all Georgians, particularly those in rural and underserved areas of the state. The center will also train future physicians and prepare them to provide telehealth-related patient care.
“We’re not identifying individual patients with this analysis, but it allows you to see the power in population health and paints a larger, higher-level picture,” MacKinnon said. “If you score lower on these two health indices and then lower on the social vulnerability indices as well, it shows a lot about an area. High-speed internet is no longer just something that’s nice to have — it’s a necessity. You can even go as far as seeing how that affects education and how that in turn can affect change and policy.”
 Augusta University
Augusta University