Whether elevated blood pressure early in life translates to increased risk of dementia is a question scientists are working to answer.
“Dementia is not a normal part of aging, and once it begins you can’t reverse it,” says Dr. Shaoyong Su, genetic epidemiologist at the Georgia Prevention Institute at the Medical College of Georgia at Augusta University.
“It typically surfaces at about age 65 or older but we think the problem really starts much earlier,” Su says of a condition characterized by loss of memory that can surface with forgetfulness and progress at varying speeds to the point of dysfunction.
There are many dementia risk factors, most of which also are known risks for cardiovascular disease, including high cholesterol and blood pressure, stiffening arteries, obesity and simply getting older.
But Su and his MCG colleagues appear to be the first to specifically explore whether a higher or more rapidly increasing blood pressure in childhood helps set the stage as higher pressures lead to vascular damage resulting in less blood flow and likely, eventual brain cell damage in some areas.
Dementia already affects about 50 million people worldwide and there are some 10 million new cases each year, according to the World Health Organization. The increasing occurrence in children of related risks, like high blood pressure — conditions previously largely relegated to adults — has enhanced the timeliness and import of finding an early way to identify those most at risk and intervene, say Su, principal investigator on a new $3 million grant from the National Heart, Lung and Blood Institute designed to help do that. So have realties of an increasing lifespan — 78.7 years— and lack of effective dementia treatment, the investigators say.
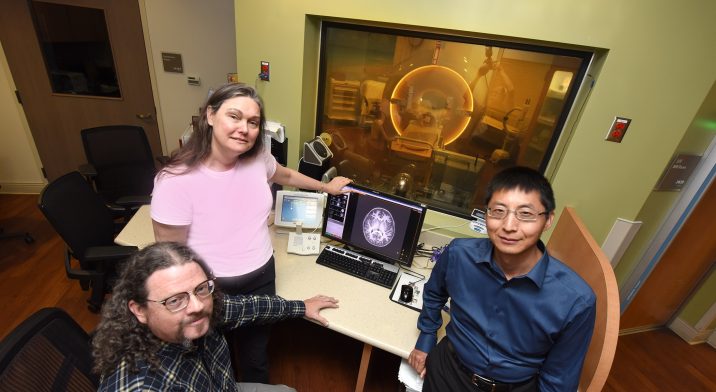
In fact, when asked if they think we are facing a dementia epidemic, Su along with coinvestigators Drs. Catherine Davis, clinical health psychologist at the Georgia Prevention Institute, and Nathan Yanasak, magnetic resonance imaging scientist in the MCG Department of Radiology and Imaging, respond in unison that we are.
So they are looking again at 600 people — about an equal number of blacks and whites, males and females — who are just reaching into midlife but on whom they have data from childhood. The individuals, now an average of 40 years old, have had comprehensive data collected up to 16 times over 23 years, including measures like ambulatory blood pressure, arterial stiffness and other measures of chronic stress and lifestyle. Like the general population, about one third of the group are now hypertensive.
This time investigators are doing painless, sophisticated brain imaging to look at relevant factors like cerebral blood flow as well as cognitive testing as a check of their brain health.
They want to answer questions like whether the arterial stiffness and even atherosclerosis they have already identified in the vasculature of some of these still-young individuals are associated with unhealthy structural and functional changes in the brain as they now reach into midlife.
“First we have to know exactly what is happening,” says Yanasak. “Once we know what is happening, we can start searching for solutions.”
“We will be able to look at associations between their cardiovascular measures over time and the current status of their cognitive ability, their cerebral blood flow and brain structure,” says Davis.
They already have some evidence that an elevated blood pressure — whether from childhood trauma, obesity or lifestyle factors like diet and inactivity — begins to affect blood flow and alter the delicate architecture of the brain.
“Decreases in flow are going to lead to increases in the probability of something bad happening,” says Yanasak, using the analogy of irrigating a growing field and knowing that if the spigot gets turned off, or even significantly down, damage will happen.
In the case of dementia, it’s not instantaneous damage, rather progressive problems. Studies already have associated, for example, hypertension in middle age with cognitive decline in old age, says Su.
Noninvasive magnetic resonance imaging, or MRI, studies, they are now using to see what is happening in these study participants’ brains include arterial spin labeling and diffusion tensor imaging.
Arterial spin labeling, regularly used to rapidly assess brain blood flow in stroke patients, tells them how much blood is flowing — or not — in the brains of the study participants, Yanasak says. The scanner basically enables you to measure blood flow through miniscule capillaries that feed brain tissue by knocking out the magnetic properties of blood, so that area goes dark on the scan and you can tell what blood flow looks like.
Diffusion tensor imaging enables a perspective on the white matter, the nerve fibers, or axons, which, much like a spark plug and its wires, enable communication between neurons, neurons and muscle cells and even neurons and other organs. These advanced scans utilize the natural flow of water to examine the integrity of neural fibers. Subtle change in this tissue, which is likely not detectable by a standard MRI, is an early sign that the fragile, minute vasculature of the brain is being impacted by high blood pressure in the body, Yanasak says. The technique, which is also used in brain cancer, already has been used to associate decline in executive function with white matter changes.
Investigators are assessing cognitive health with tests like the antisaccade task, which requires participants to look in the exact opposite location to a stimulus, resisting the natural urge to look at the stimulus.
To continue to assess lifestyle, participants are answering questions like how many days a week they do physical activity sufficient to work up a sweat, and how often they smoke and drink alcohol. The investigators are then looking to see whether unhealthy environmental factors correlate with higher blood pressure and worsen any impact on the brain and cognition. “We can see whether their lifestyle can influence or modify the relationship between blood pressure and brain cognitive function,” Su says.
Participants’ stress levels also are again being assessed by answering questions about problems like stress within their family or neighborhood or work, as well as adverse childhood events and socioeconomic status. Traumatic childhood experiences, like sexual assault or abandonment, can result in actual structural changes to a child’s developing brain and put them at increased risk for unhealthy habits like smoking and other substance abuse, Su says.
Now the researchers want to know more about that and the impact of chronic stress as well as we age. Current measures will be compared to similar ones taken over the past 23 years to get better insight into major stress factors across some 40 years of life, Su says.
They also are looking at whether ethnicity and sex are factors in providing protection or increasing these unhealthy associations. There are already some established associations, like black males tend to have higher blood pressure earlier in life, including a significantly higher nighttime blood pressure. Again, says Su, they want to see if these sex and ethnic differences also translate to a different dementia risk and the need for different strategies and times to intervene or treat the problem.
It’s established that elevated blood pressure in the body can lead to damage in the arteries of both the body and the brain. Associations already have been made in the longtime study group between an elevated resting blood pressure and a larger left ventricle, the pumping chamber of the heart. Increases in the size and possible eventual dysfunction of the ventricle correlate with the muscle having to work extra hard against higher pressure inside blood vessels. Associations between high blood pressure at middle age and dementia have been made by studying executive function, things like concentration, attention and working memory, which, as the name implies, enables us to do things like problem solve and make decisions.
The investigators suspect they will also find that at this entry point to midlife — midlife is considered to be from about ages 40 to 65 — brain changes that may later surface as dementia.
Among the same group of individuals, Su reported in 2015 in the journal Circulation that those who experienced multiple traumatic events, from emotional and sexual abuse to neglect, in childhood had higher blood pressures as young adults than their peers. The difference of 10 points in the systolic pressure — the top number denoting pressure while the heart is contracting — by early adulthood puts these young people at higher risk for hypertension and coronary artery disease by middle or old age.
Alzheimer’s and vascular dementia are the most common dementias.
Dr. Jennifer McDowell, cognitive neuroscientist who is chair of the University of Georgia Behavioral and Brain Sciences Program, is co-principal investigator on the new grant.
 Augusta University
Augusta University