Blake McGee, PhD, chair of Augusta University College of Nursing’s prelicensure department, has been accepted for publication in Blood Advances. The American Society of Hematology’s journal has selected his manuscript, Changes in Acute Care Use Among People with Sickle Cell Disease After Adoption of a Prescription Drug Monitoring Program.

Georgia State University provided funding to McGee to work with the Sickle Cell Data Collection program in studying how various policies affect pain management equity among those with sickle cell disease. Emergency department visits and the prescription of opioids play a critical role in the management of sickle cell, especially for those in a vaso-occlusive crisis. However, due to the opioid crisis, there has been a culture shift toward a more cautious use of opioids, with many states implementing prescription drug monitoring programs to track the distribution of opioids.
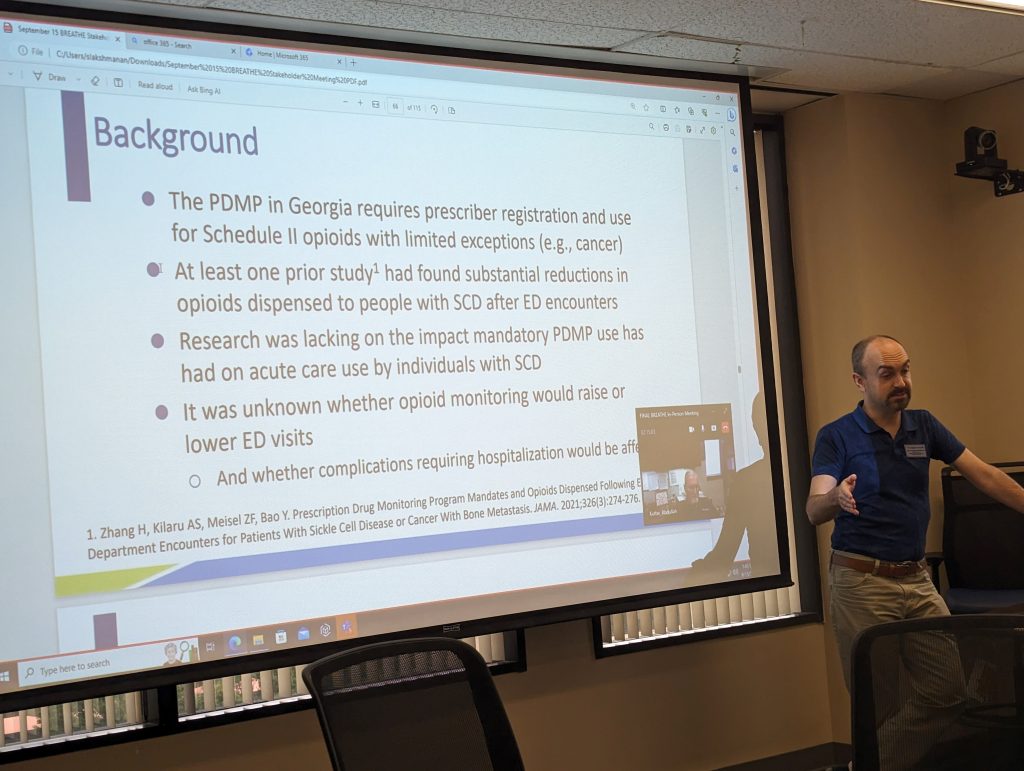
When starting their research, McGee and his associates noticed limited studies on the unintended or adverse outcomes of prescription drug monitoring programs. However, a single existing full-fledged research publication did find that those with sickle cell disease had experienced a reduced prescription of opioids at discharge.
This sparked questions for McGee and his colleagues. Is there an association that can be observed between the implementation of state prescription drug monitoring programs and acute care use for those with sickle cell disease? Would prescription drug monitoring programs curtail access to pain medication, therefore spiking emergency department visits? With these questions in mind, his team decided to measure the net effect of prescription drug monitoring programs in Georgia.
“What we noticed was that emergency room use by those with the disease really declined after prescription drug monitoring programs started in Georgia,” said McGee. “While it is not determined whether the decreased volume of emergency room usage is a positive or negative side effect, we do know that this is a disease where it is often medically necessary to go to the emergency room.”
In a parallel study performed with aggregate data from the Georgia Department of Public Health, the team looked at the trends in opioid fulfillment among people with sickle cell, against those in the general population, over a five-year period in Georgia. They observed that those with sickle cell disease were filled with a longer day supply of medication on average, which could provide one explanation for the decrease in emergency room visits.
The findings of this observational study led to further questions about the impact of opioid policies on this vulnerable population. Those with sickle cell disease are not documented as overusing or misusing opioids at higher rates than other populations, and other factors like the majority ethnicity of the sickle cell population could also play a concern in health equity.
For many states, diseases like cancer are exempt from prescription drug monitoring program requirements, and some have been considering adding sickle cell disease to the exemption list. McGee and his team are hopeful that the results from their study could influence more states to consider adding sickle cell to the exemption list, therefore preserving the quality of care that those with sickle cell receive.
 Augusta University
Augusta University




