It’s the proportionality of a newborn — a measure that includes both birthweight and length — that may best tell doctors whether a child is born with an increased risk for heart problems later in life, investigators report.
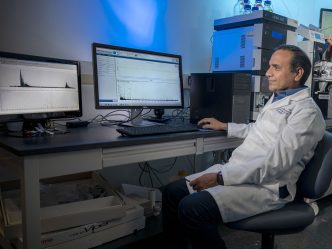
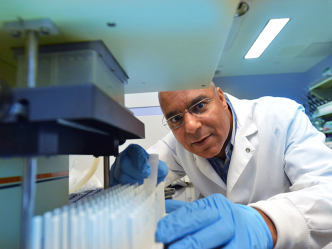
Birthweight, while important, tells only part of the story of fetal growth, while the additional consideration of length, gives a more complete picture of both fetal growth and growth trajectory, says Dr. Brian Stansfield, neonatologist at the Medical College of Georgia and Children’s Hospital of Georgia at Augusta University.
Measures called ponderal index, or PI, as well as the more widely used body mass index, or BMI, which both account for height and weight, likely provide a more accurate indication of fetal growth and what’s ahead for the child, says Stansfield, corresponding author of the study the journal Early Human Development.
The new study indicates that a low PI or low BMI at birth, much like high cholesterol or high blood pressure, should be considered a risk that needs attention and intervention, says Stansfield who is also a research clinician in MCG’s Vascular Biology Center.
Historically, birthweight has been the focus of studies connecting early life to later health consequences.
“When you look at birthweight alone, you are looking at a measure at a single point in time, which is a big problem when it comes to projecting out,” says Stansfield.
It’s known that perinatal growth — which is affected by numerous factors from genetics to environmental ones like the mother’s health and habits like smoking, nutrition and gestational diabetes — has important implications for heart development, and animal and human studies have associated low birthweight with heart problems and death.
MCG investigators hypothesized that a baby’s PI or BMI at birth would provide a much better indicator of heart development and future function than just birthweight.
They found in a group of 379 healthy adolescents, that a low PI — where increases in height and weight are out of sync during development — was most associated with an increase in the size of the major pumping chamber of the heart, the left ventricle, which is considered a risk for future cardiovascular disease.
The findings further suggest that factors that impact fetal growth also can alter heart development, changes that may have a permanent, negative impact on heart function and cardiovascular health as adults, they write.
They also indicate that proportionality can help differentiate babies who are born small because of their genetics — smaller parents tend to have smaller babies, for example — and those who fail to reach their in utero growth potential for other reasons.
“What we are trying to do is understand how do we categorize these children at birth so that we know who to watch more closely and ideally intervene earlier to help offset some of these risks,” Stansfield says.
While his study found that a low PI had the highest association with risk factors for heart problems, the more widely used BMI is also a good tool, he notes. BMI accounts for length, by dividing birthweight by birth length to the second power, while PI gives length even more emphasis by using the power of three.
“We believe our findings are a call to pediatricians to be even more diligent in measuring and noting birthweight and length parameters,” Stansfield says of his typically exceedingly thorough colleagues. They also are a call to adult primary care providers to be aware that this very early measure of height and weight can provide lifelong insight into an individual’s risk of heart and other disease, he says. Digital health records should help doctors and patients alike find and keep up with these early statistics and ideally intervene before trouble starts, he notes.
Additionally, they are another reminder to mothers-to-be to abstain from smoking, alcohol and drugs; eat right; and exercise safely during pregnancy to try to ensure a healthy environment for their developing child, Stansfield says. He notes that even the genetics a baby inherits can be altered for better or worse through what he experiences during development.
Risks for health problems like heart disease are a confluence of genetics and environmental risks and those environmental risks also start in utero, he says.
For this study, they looked at 379 healthy black and white adolescents ages 14-18 from the Augusta, Georgia area. Parents provided their children’s birthweight and length, which were used by investigators to calculate a BMI and PI.
Two-dimensional echocardiography was used to noninvasively look at the children’s left ventricle for telltale indicators of hypertrophy like thickening of the walls and less blood being pumped out.
Then, in what appears to be the first study to do this, they looked at relationships between birthweight and birth BMI and PI and the structure and function of the left ventricle in the children.
Other measures also were done, like the Tanner scale, which looks more specifically at pubertal development. The investigators also assessed factors like socioeconomic status and physical activity, including the children wearing monitors to track physical movement for seven days.
Stansfield notes that at the time of their follow up for this study, about 25% of the adolescents had obesity or were overweight and most were on an upward trajectory with their BMI, which is not good.
Children with an upward trajectory had about a 30% likelihood they would become obese versus those with a downward trajectory, who have about a 5% likelihood.
There was also about a 40% increase in visceral adiposity — fat around the belly and the organs inside the abdominal cavity, which is considered particularly unhealthy — in adolescents with the upward versus downward BMI trajectory. Those children also were much more likely to have a higher systolic pressure — the top number of a blood pressure which indicates the pressure inside arteries when the heart is contracting.
While more work is needed to put all the pieces together, proportionality also may help identify babies who appear, at least at birth, to be headed toward good heart health, Stansfield says.
Lab animal studies indicate that cardiac mass is mostly determined at birth, and production of heart cells, or cardiomyocytes, that make up the heart rapidly diminishes after birth so, to get larger, the heart cells you are born with have to enlarge, called hypertrophy, which is not considered normal growth. Enlargement of the left ventricle typically results from the heart having to work too hard against, for example, high pressure inside blood vessels, and can result in heart failure.
MCG investigators reported last year in the journal Pediatric Research that fetal growth restriction in Guinea pigs suppresses the production of and increased the death of cardiomyocytes, and led to hypertrophy of cardiomyocytes that were present and other disruptions of the heart’s normal architecture.
The risk of other chronic disease, like obesity and diabetes, also has now been linked to low birthweight but the cardiovascular system seems particularly impacted by perinatal growth, the investigators say. In fact, by week five, the baby’s heart has begun to develop, and it’s during this critical period of development that the baby is most at risk for birth defects from factors like alcohol consumption by the mother and some medicines.
The research was supported by the National Institutes of Health, the American Heart Association and the U.S. Department of Defense.
 Augusta University
Augusta University