As the name implies, induced pluripotent stem cells can become any type of cell in our body, and scientists have evidence that when they prompt them to become muscle progenitor cells they can help restore the sometimes debilitating muscle loss that happens with age.
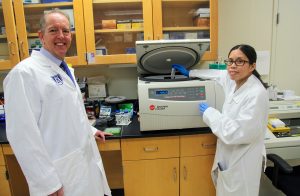
Progressive, age-related muscle loss is called sarcopenia, and it can impair mobility and quality of life, says Dr. Wanling Xuan, stem cell biologist in the Vascular Biology Center at the Medical College of Georgia.
Muscle supports the skeleton and enables movement, and the loss of muscle size and strength increases falls, hospital stays and recovery times, which can result in even more muscle wasting, disability as well as premature death, says Xuan. Sarcopenia also can contribute to diseases like obesity, osteoporosis and diabetes, drive health care costs up and quality of life down, according to the Alliance for Aging Research.
“We want to help people who are suffering with this situation,” Xuan says.
She has evidence that one of the most efficient and effective ways to do that is by using a small manmade molecule called givinostat to coax the induced pluripotent stem cells, or iPSCs, to become these muscle, or myogenic, progenitor cells. These cells make actual muscle cells as well as the extracellular vesicles — little nearby containers packed with muscle-specific cargo, like microRNAs — that aid muscle repair and regeneration.
Xuan is principal investigator on a $1.6 million grant (1RO1AG070145-01) from the National Institutes of Health to further explore the benefit of directly administering these myogenic progenitor cells or the extracellular vesicles they produce.
In their animal model of aging-related sarcopenia, they’ve already shown the strategies increase the number of muscle stem cells and decrease destructive inflammation, which typically increases with age.
Givinostat, which is in the final phase of clinical trials for muscular dystrophy, is a manmade small molecule that inhibits HDACs, enzymes that help turn genes off, and can steer iPSCs to become muscle progenitor cells and muscle-specific extracellular vesicles. Other small molecules produce less-specific cargo, Xuan says.
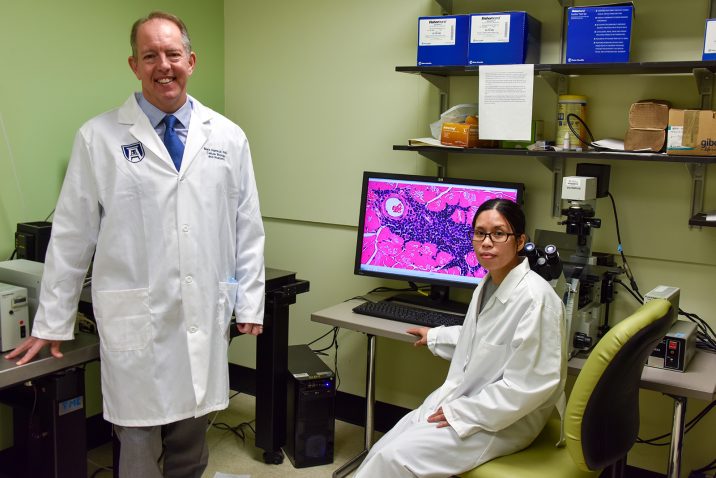
“Givinostat primes them, it tunes them to produce the right type of vesicles,” says coinvestigator Dr. Mark Hamrick, a bone and muscle biologist in the MCG Department of Cellular Biology and Anatomy and MCG’s senior associate dean for research.
Xuan already has identified some of the cargo, including mRNAs that activate cell signaling pathways important to muscle regeneration.
Since giving the entire iPSC could result in tumor production, Xuan thinks and has early evidence that for strictly age-related muscle loss, just giving the vesicles produced by her process is likely the best strategy — and medicine — to help regenerate aged stem cells and restore more resilient, youthful muscle. In fact, many of the regenerative properties of muscle progenitor cells can be credited to the vesicles, Xuan says.
She suspects that in older individuals who have an actual muscle injury in the face of sarcopenia, giving the muscle progenitor cells themselves may be a better option, because of the individual’s impaired ability to generate new muscle cells that may be needed for a full repair. She notes that in the high oxidative stress environment of aged or diseased muscle, it can be hard for new muscle cells to integrate and become helpful, which is another avenue they are exploring.
When we are younger, skeletal muscle stem cells called satellite cells hovering in the vicinity of our muscles, produce most of the muscle progenitor cells and extracellular vesicles in response to exercise or injury. But the function and number of satellite cells decline with age, likely starting in our 40s, Hamrick says.
The cargo vesicles carry also likely changes in response to an aging environment like the increased levels of destructive factors such as inflammation and oxidative stress, Hamrick says. Also with age, some cells become senescent — not dead but also not carrying out their usual function — and there is increasing evidence these “zombie” cells are producing damaging factors as well, Hamrick says.
Muscle wasting diseases like muscular dystrophy also decrease the number and function of satellite cells, and the scientists have evidence their technique may help there as well.
Xuan and longtime mentor Dr. Muhammad Ashraf, professor and stem cell biologist in the Vascular Biology Center, have a new paper in the journal Stem Cell Research & Therapy indicating that using givinostat to induce iPSCs into action helps replenish satellite cells in the face of muscular dystrophy. The technique also produces a lot of muscle-making progenitor cells as well as new blood vessel growth to sustain new muscle following muscle injury in a muscular dystrophy animal model. It also restores levels of dystrophin, a key protein for the muscle that supports the skeleton that is missing in muscular dystrophy, they report.
The scientists say that their rejuvenating approach likely could be applied to other conditions as well, including any aging cell type, and that giving extracellular vesicles already is being explored for stroke recovery and bone repair, Hamrick notes.
There is a lot of individual variability in the amount of muscle loss we experience with age — more active individuals tend to have less, while inactivity and disease can accelerate loss, Xuan says
Sarcopenia produces changes like atrophy of fast-twitch fibers, the fibers that generate muscle’s speed and power, Hamrick says, one of the reasons falls become more likely.
“People don’t have the capacity to quickly move, catch themselves, prevent the fall,” he says. Fat also accumulates in previously lean muscle, which can affect its look and function. The point of communication between muscles and the nerves that tell them what to do also degrades.
While some treatments, like growth hormone supplements are under study, exercise like resistance, or strength, training and a healthy diet are your best sarcopenia prevention options, Xuan says. In fact, there is evidence in humans that resistance training improves stem cell proliferation — and so muscle regeneration — and increases the size of fast-twitch muscle fibers, Hamrick says.
 Augusta University
Augusta University