AUGUSTA, Ga. – A recent study of a handful of patients supports mounting evidence that targeted suppression of inflammation packaged with standard therapy can improve the cognitive ability of patients with schizophrenia, physician-scientists report.
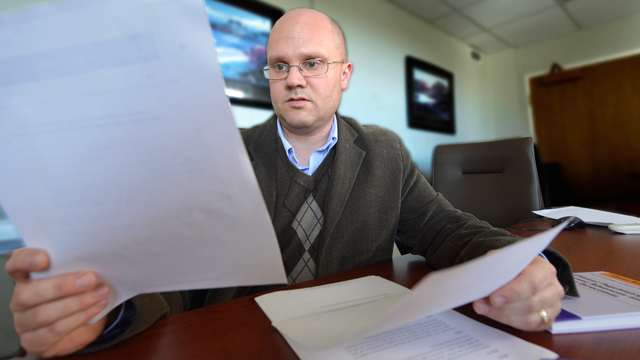
After just two intravenous doses in eight weeks of tocilizumab, an immune-suppressing drug regularly prescribed for rheumatoid and juvenile arthritis, study participants had significantly improved cognitive ability, said Dr. Brian J. Miller, a psychiatrist at the Medical College of Georgia at Augusta University.
“This adds to the growing evidence that inflammation plays a role in patients with schizophrenia and again suggests that targeting inflammation may be a viable therapeutic target, at least for cognitive impairment, which is a huge area of unmet need,” Miller said.
Cognitive problems typically are a major source of dysfunction and disability in these patients and can be among the earliest symptoms of schizophrenia, said Miller, corresponding author of the report in the Journal of Clinical Psychiatry.
Anywhere from 25 to 50 percent of patients may have inflammation in the brain contributing to that dysfunction. Problems range from having trouble remembering important numbers to impairment of executive function that enables them to analyze, organize, and generally manage their lives.
Tocilizumab targets the receptor for IL-6, a protein which helps regulate inflammation that is often elevated in patients with schizophrenia. Higher IL-6 levels also have been correlated with a smaller hippocampus, a center for learning and memory in the brain, as well as experiencing more psychiatric symptoms.
The five study patients did not experience improvement in overall levels of psychiatric symptoms, such as hallucinations and delusions, more classic symptoms of schizophrenia, which were already well- controlled with antipsychotics, Miller said.
Nonsteroidal anti-inflammatory drugs, including aspirin, have been tried in these patients, but tend to be less potent and have multiple mechanisms of action, Miller said. “If we see improvements with this drug, then we know it’s not due to other effects.”
Increasing evidence of inflammation’s role in schizophrenia, means that Miller already routinely tests his patients’ blood level of C-reactive protein, an indicator of inflammation and IL-6 levels, and he may try a variety of anti-inflammatory drugs in addition to an antipsychotic.
While he did not pretest in these study patients, Miller later learned that while all appeared to benefit from the targeted anti-inflammatory therapy, only half had elevated C-reactive protein level. That finding is another reason a larger, double-blind study is needed, he said.
While given intravenously for the study, a newer injectable version of tocilizumab also is now available, Miller said. Drugs that directly target IL-6, rather than its receptor, are now available as well and Miller recently received a grant from the nonprofit Stanley Medical Research Institute to examine the effectiveness of one of these drugs, siltuximab, in patients with blood evidence of inflammation. Since he already sees most of his patients monthly, giving these types of drugs should not be much of an additional burden for them.
The tocilizumab study was funded in part by an American Psychiatric Association Kempf Fund Award for Research Development in Psychological Psychiatry.
 Augusta University
Augusta University