Cisplatin is a common, powerful chemotherapy agent used for a wide range of cancers such as breast, ovarian and lung, that in a handful of days can also permanently damage or destroy patients’ kidneys.
Now researchers want to turn the tide by protecting the kidneys while improving cisplatin’s efficacy against cancer.
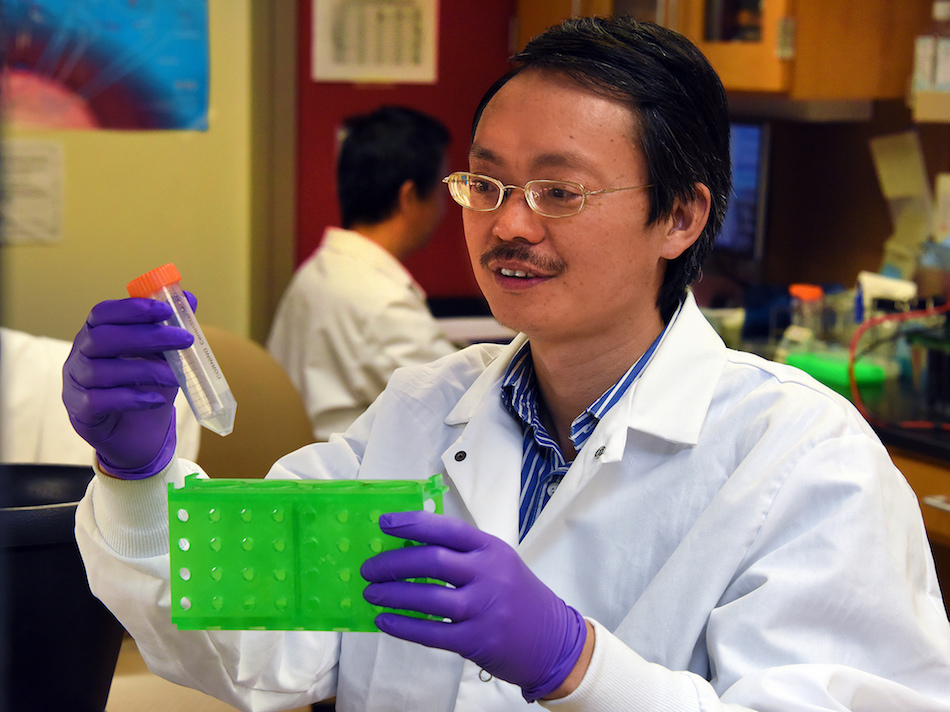
“There is no question that cisplatin is a very important chemotherapy drug,” said Dr. Zheng Dong, cellular biologist and Regents’ professor in the Department of Cellular Biology and Anatomy at the Medical College of Georgia at Augusta University. He’s principal investigator on a renewed $1.5 million grant from the National Institute of Diabetes and Digestive and Kidney Diseases that could ultimately make it even better.
More than 25 percent of patients treated with cisplatin develop kidney problems; their kidney recovery hinges on variables such as what cisplatin dose they took for how long and the severity of the initial kidney injury.
It’s a well-known consequence that has even sent researchers looking for analogues that are safer for the kidneys, but those have ultimately been less effective cancer fighters, Dong said. Excessive hydration during therapy has not made much of a dent either. Cisplatin’s impact also is not hugely surprising since the fist-sized kidneys – which filter about 120-150 quarts of blood daily and produce 1-2 quarts of urine – reabsorb about 99 percent of what they filter.
“You can get toxic compounds also reabsorbed into the kidneys,” Dong said. “A large portion of patients end up with renal failure.” Interestingly the inner ear also can be, most typically transiently injured by cisplatin.
In about a dozen years studying the untoward impact, Dong’s research team has found cisplatin causes DNA damage – a huge stressor for the kidney cells. That response includes increased activation in the kidney of the tumor-suppressor gene p53. P53 prevents damaged cells from dividing, which is what happens in cancer, and one way cisplatin attacks cancer. It can also prompt badly damaged cells to commit suicide and ultimately provide space for cell regeneration and kidney repair.
A second cisplatin-related kidney cell injury/death pathway his lab identified is PKCδ, a member of a large class of proteins known to change the function of other proteins by adding phosphates. With cisplatin treatment, PKCδ also becomes overactive. “We don’t know under normal conditions what PKCδ does. But we know when the kidneys are in trouble, it’s activated and cisplatin activates it,” he added.
“We have the p53 pathway. We have the PKCδ pathway. They both contribute to kidney cell death during cisplatin treatment. The question is: how do they do it?” Whether they act synergistically, as he suspects, or independently, are some of the questions he wants to answer. Whether overactive PKCδ makes normally helpful protein harmful is another.
In this scenario, P53 and PKCδ appear to balance each other out by respectively inducing and suppressing autophagy in response to cisplatin. Autophagy is essentially cannibalism, where a cell consumes its damaged portion with the goal of repair and survival. Dong prefers the metaphor of pulling weeds in a garden. “Autophagy, I always believe, is at least initially, not about death, but about survival.”
He knows that the initial response of a cell under stress is to survive and, in this case, autophagy can help the kidney cell eliminate its own damage. Selective weeding includes mitophagy, which is eliminating damaged cell powerhouses, which Dong thinks also ultimately protects the kidney. Damaged powerhouses can actually produce substances that kill kidney cells, while their death can result in powerhouse regeneration.
Dong is betting that if he can inhibit PKCδ, he can augment kidney-cell survival and cancer-cell death. No doubt p53 is bad for the kidney and for cancer, so he wouldn’t want to inhibit it unless that could be done only in the kidneys. But PKCδ is bad for kidneys and good for cancer. “If we can inhibit it, we may be able to save the kidneys and help kill the cancer,” Dong said. His new studies include looking at the effects of PKCδ inhibition in autophagy-suppressed and non-suppressed mice.
The ultimate goal of Dong and his colleagues is better understanding if and how P53 and PKCδ interact with each other and with autophagy and how they can potentially augment autophagy to help kidney cells survive rather than die from the stress of cancer therapy. “We want to increase or activate the protective mechanism and to suppress the cell-death program for the kidney at least,” Dong said.
While patients may need cisplatin for months, the kidney damage can occur in the first few days of use. Initially it may cause severe kidney dysfunction, a sub-lethal injury that may not directly kill kidney cells but dramatically reduces their function. In severe cases, no urine is even produced. Either way, patients may develop some residual damage so their kidneys don’t function optimally.
Dong is also senior career research scientist and director of research development at the Charlie Norwood Veterans Affair Medical Center in Augusta.
 Augusta University
Augusta University