Scientists want to know whether our aging fat cells are important to the onset and progression of Alzheimer’s.
They have evidence that as we age, our fat becomes less efficient at producing a hormone that helps support the growth and survival of neurons and helps regulate their activity. The result can be neurons in areas of the brain important to learning and memory become dysfunctional, degenerate and we develop Alzheimer’s.
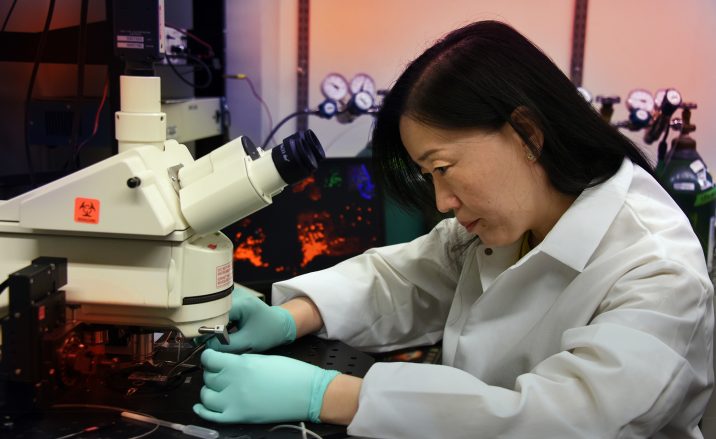
“What happens to neurons, that is really what we are interested in,” says Dr. Xin-Yun Lu, molecular behavioral neuroscientist at the Medical College of Georgia at Augusta University and Georgia Research Alliance Eminent Scholar in Translational Neuroscience.
Lu is principal investigator on a $3.5 million grant from the National Institute on Aging at the National Institutes of Health that is helping further explore the possibility that improving the function of our older fat may just help our brains.
The hormone adiponectin, which is made by fat cells, circulates in our blood and enters our brain. Inside fat cells, its production is regulated by peroxisome proliferator-activated receptor gamma, or PPAR-ƴ, a transcription factor that’s essential for early stage fat cells to become mature, fully functioning ones.
“We know when you have Alzheimer’s, your adiponectin is low; now we want to make sure this is actually a cause,” Lu says.
Both adiponectin and PPAR-ƴ have been implicated in Alzheimer’s and delivering adiponectin to the brain has been shown to improve cognition in a mouse model of Alzheimer’s. PPAR-ƴ agonists, which increase adiponectin levels, already are used to lower cholesterol and blood glucose levels and have been tried in Alzheimer’s as well.
However, investigators studying the agonists’ potential in Alzheimer’s have reported difficulty with the drugs reaching the brain, and that the high doses needed to compensate for that result in side effects like edema, heart failure, liver abnormalities and weight gain. These findings have some calling for more selective PPAR-ƴ therapies.
Lu has evidence that for Alzheimer’s, that could mean targeting PPAR-ƴ2, the version of PPAR-ƴ primarily made by fat cells. The other, PPAR-ƴ1, is the target of current PPAR-ƴ agonists, says Lu, and can be made by a variety of cells in other organs, such as the heart and kidney, which could account for the undesirable side effects.
In the search for a better solution, the grant is enabling Lu and her team to further explore the relationship between adiponectin made by fat cells and the cognitive decline that comes with aging. They also are looking at the receptors for adiponectin on neurons in centers of learning and memory in the brain to explore their distinct function, what happens to them with the onset and progression of Alzheimer’s and the vulnerability of the neurons with the receptors to degeneration.
Lu’s team thinks the benefit of PPAR-ƴ agonists in Alzheimer’s results from activating the PPAR-ƴ in fat cells, which increases adiponectin production, so they are using mice missing PPAR-ƴ in adult fat cells to look at its effects on cognition, metabolic function, the overall health of neurons and the hallmark neuropathological lesions in a mouse model of Alzheimer’s.
Obesity researchers made the connection between fat cells, PPAR-ƴ and adiponectin, notes Lu. Interestingly, in obesity, fat cells become less efficient at making adiponectin, which is anti-inflammatory and can help regulate neuronal activity, including turning activity of some neurons up and others down. One theory is that fat cells instead start making inflammation-promoting signals called cytokines and inflammation hinders adiponectin production, so neurons suffer.
The same thing essentially happens with age, which is Lu’s focus, and when Alzheimer’s tends to occur. Fat stores begin to shift from beneficial subcutaneous fat to unhealthy fat that piles up on our bellies and around the organs inside our abdominal cavity, producing a hotbed of inflammation and a lot less adiponectin.
It’s not really about how much fat you have but what kind of fat cells you have and what hormones those fat cells can make, Lu says, that may affect your risk of Alzheimer’s.
“Your fat cells were making beneficial adipokines like adiponectin, which decrease inflammation, and now are making more proinflammatory cytokines,” she says. This shifting toward unhealthy fat is a natural one that occurs regardless of your body weight, she notes.
In the brain, adiponectin has two distinct receptors on neurons, AdipoR1 and AdipoR2. Lu’s lab has found that activating adiponectin receptor 1 and disrupting adiponectin receptor 2 increases the excitability of neurons in the hippocampus while disrupting receptor 1 and activating receptor 2 decreases it.
Excessive excitability is common in early stages of Alzheimer’s and leaves neurons vulnerable to degeneration. And Lu thinks Alzheimer’s also manipulates this pathway to alter and ultimately decrease neuron function in the brain’s cerebral cortex and hippocampus, centers of learning and memory, that are heavily hit by Alzheimer’s, the most common dementia.
They have shown that before they die, neurons become hyperactive and generally don’t function well. In fact, patients as well as animal models of Alzheimer’s can experience seizures, a sign of excessive excitability.
“When you have Alzheimer’s, you have neurons die in the cortex and the hippocampus,” Lu says. In fact, the brain generally shrinks in size. Why some neurons die and others don’t is what Lu and her team are trying to better understand.
Now they are working to better understand the functions of the apparently distinctive receptors, particularly on the neurons that produce glutamate, a brain chemical that helps excite cells and is known to be critical to cognition.
They suspect the receptors’ clearly opposite effects on cell excitability could mean they also have a different, and possibly opposite as well, effect on Alzheimer’s development. So they are looking at what deleting and activating the receptors does to those neurons and what that does to contribute to or alleviate age- and Alzheimer’s-related changes to the brain and our ability to think and remember.
They also are studying what happens to the receptors themselves in different age mice.
Adiponectin has a protective, or neurotrophic, effect on neurons, helping enable their survival, growth, repair and even regrowth. They can help neurons and their connections stay nimble, or plastic, so our brains function better, and we can continue to properly respond to our environment and maintain other brain basics like making memories.
Genetic variations in PPAR-ƴ and adiponectin as well as low blood levels of adiponectin already are associated with an increased Alzheimer’s risk. In fact, low adiponectin levels in the cerebrospinal fluid in the brain have been associated with increased production of the hallmark plaque and shrinking of the hippocampus associated with Alzheimer’s.
Alzheimer’s is the sixth leading cause of death in the United States, according to the Centers for Disease Control and Prevention. First symptoms may appear after age 60 and the number of people with it doubles every five years beyond age 65, according to the CDC. It’s known that metabolic disorders, like obesity, cardiovascular disease and diabetes, increase Alzheimer’s risk. In fact, Alzheimer’s is sometimes referred to as type 3 diabetes, which is thought to result from resistance to insulin in the brain.
Lu also studies adiponectin in depression and has shown how chronic stress can decrease fat’s production of PPAR-ƴ and adiponectin.
 Augusta University
Augusta University