For years, Georgia has consistently been ranked as one of the most dangerous states in this country to be a new mother.
Approximately 26 Georgia women die from pregnancy complications for every 100,000 live births, compared to the national average of about 17 women. But even more devastating is the fact that about 60% of the state’s maternal deaths between 2012 and 2016 were found to be preventable, according to the Georgia Department of Public Health.
And the mortality rates are much more tragic for Black women in Georgia. African American women are almost three times more likely to die from a pregnancy-related cause than white women in Georgia. Black mothers in rural areas of Georgia are at an even higher risk.
The leading causes of pregnancy-related deaths in the state involve cardiomyopathy, cardiovascular or coronary conditions, hemorrhage, pulmonary embolism, preeclampsia and eclampsia. Many of the fatalities happen not during childbirth, but in the months following due to factors like postpartum depression, high blood pressure and cardiac conditions, according to the Georgia Department of Public Health.
Dr. Raeonda Bullard, a third-year resident physician in the Department of Obstetrics and Gynecology at the Medical College of Georgia, is in the unique position to see both sides of this crisis. Not only does she regularly treat pregnant patients facing some of these same conditions, but she, herself, is a new mother of a beautiful baby boy.
“As a minority, I can honestly say that I think there’s a lot of distrust in our community with health care,” said Bullard, who grew up in the Atlanta area. “Some people just don’t trust doctors. In fact, my mom has a daughter and a son-in-law who are doctors, and she still does not trust a lot of what doctors say. There’s nothing that the doctors have specifically done, it’s just how we grew up.
“I think health care providers have to be aware of that bias. So, when a doctor walks in the room, it may take an extra minute for them to connect with the patient if they don’t look like that patient.”
Building an open and honest relationship with the patient can make all the difference in the world by drastically improving the care that individual receives, Bullard said.
“That extra two-minute conversation lets the patient know that they can trust you and the next thing you know, they may say, ‘You know what, doctor, I’m actually worried about my blood pressure,’” Bullard said. “These are the things that you can’t see during one or two visits. You must build trust and that is one of the biggest hurdles we face that can lead to a downward spiral in a person’s future health.”
Doctors must also understand the difficult financial choices faced by some individuals in minority communities when seeking care if they don’t have health insurance, Bullard said.
“Some people in a minority community may not go to the doctor because it’s a question of, ‘Am I going to pay for a doctor’s bill when I don’t feel sick or am I going to pay to keep the lights on?’” Bullard said. “Many will obviously choose their necessities, but, unfortunately, their health issues keep perpetuating as time goes by. Then, if a woman becomes pregnant, she might also find out that she’s facing diabetes and high blood pressure. So, I think there’s a big need for preventative care.”
In fact, her own family was deeply impacted by not seeing any early warning signs of a health risk, Bullard said.
“My father passed away at 57 from a heart attack,” she said. “We never knew he was sick because he never went to the doctor. I think that’s a huge part of the problem. We need to be reaching out to communities before something happens. Start the trust early.”
Also, having more minority physicians in the health care industry can help put patients at ease when facing regular appointments, Bullard said.
“There have been multiple times where patients will say, ‘I’m so glad I have a Black doctor,’” Bullard said, laughing. “It happens the minute I walk in the room and I haven’t even said my name yet.”
In addition, becoming a first-time mother has given Bullard an entirely new perspective on the challenges for her pregnant patients, she said.
“Since having my son, I feel like I’ve changed so much. I’ve only been back to work for a few weeks, but I’ve changed as a physician just being a pregnant person,” Bullard said. “I can now relate to patients much better. I know what it feels like to be a severe preeclamptic. It definitely changes how you practice when you can connect on a personal level.
“I know I can connect with patients so easily, because I am them.”

About 10 years ago, the human rights organization Amnesty International issued a report declaring that our country was facing a “maternal health care crisis” and Georgia’s maternal mortality rate was the worst in the United States.
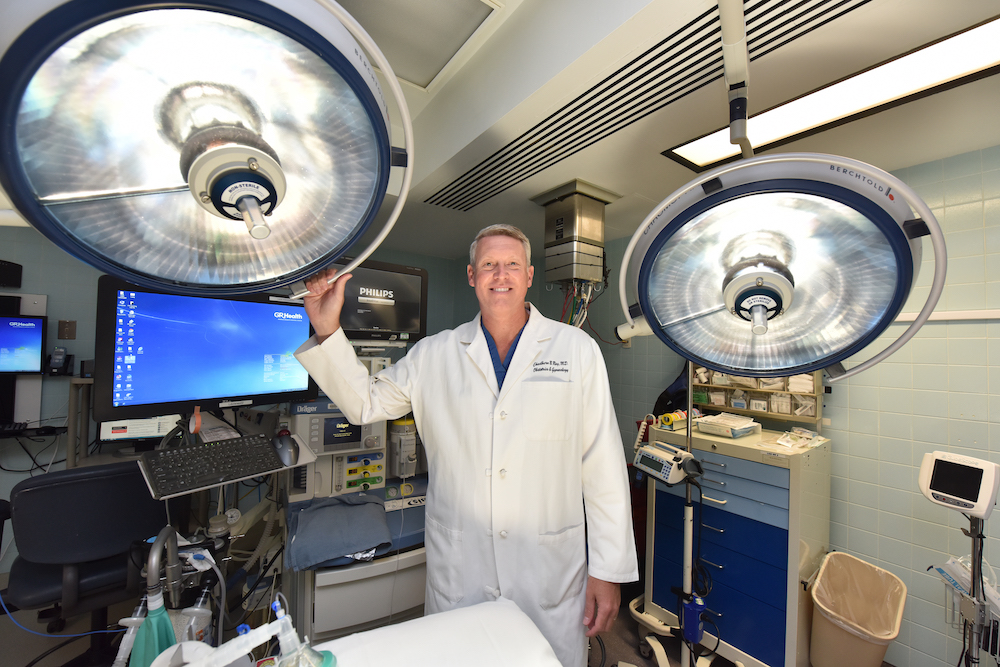
The news was devastating and led to a lot of negative press across the state, but Dr. Chadburn Ray, interim section chief of Obstetrics and General Gynecology at the Medical College of Georgia, said it also forced the medical community to take crucial steps in determining the true and accurate maternal mortality rate in Georgia.
“Maternal and infant mortality are really significant indicators of the quality of health in any area, so my colleagues around Georgia really felt challenged to do something that we hadn’t done in a long time in our state, which was to get the data,” Ray said. “Because you can’t really fix something unless you know who and why. And then you assemble the stakeholders to formulate a plan to make a dent and to move the needle on something that is just so important.”
Ray said he specifically got involved in the collection and review of the state’s data after reading an article about the East Central Region of Georgia, which highlighted an extremely high maternal mortality rate in the counties surrounding the Augusta area.
“I read the reported maternal mortality rate of the region where I worked. And, if those numbers were actually true, which they weren’t quite accurate, it would have made the East Central Region of Georgia, our health district, probably the worst or one of the worst in the entire country,” he said. “That’s when I got involved on the Georgia Maternal Mortality Review Committee and I’ve been on that committee now for about eight years. It’s one of the more gratifying things I do.”
The Georgia Maternal Mortality Review Committee identifies maternal deaths occurring during or within a year of the end of a pregnancy and reviews each case to determine pregnancy-relatedness, causes and contributing factors and to make recommendations for interventions to reduce future deaths. This multidisciplinary committee is comprised of physicians, nurses, public health workers and epidemiologists.
The review committee’s work helps the medical community look at the actual maternal deaths in Georgia, which is important because there’s a lot of differing information published about this topic.
For instance, a recent story published in U.S. News and World Report puts Georgia atop the list of states with the highest maternal mortality rates, with 46.2 maternal deaths per 100,000 live births and an even more alarming 66.6 maternal deaths per 100,000 live births for Black women.
In 2016, The Yale School of Public Health found the pregnancy-related maternal mortality ratio in Georgia was 40.8 per 100,000 live births.
Those numbers are much higher than the 26 pregnancy-related deaths per 100,000 live births reported by the Georgia Department of Public Health.
“The data that we have comes directly from the actual data from Georgia,” Ray said. “We do compare that data to the nation and we often get compared to data around the world, which I think is a little unfair because the world doesn’t count their maternal mortality rates the same way that individual states do — not always a fair comparison.”
Even each individual state has different methods in collecting their data, he said.
“So, when we talk about race and racial disparities as it relates to maternal mortality, it’s sometimes harder to actually know the number,” he said. “But it’s most commonly reported that African American women or women of color have a two to three times higher likelihood of having a pregnancy-related death than white women. And that’s something we are working to change.”
One of the major problems facing the rural areas of this region is access to health care, Ray said.
“We have a rural population outside of an urban area here in Augusta-Richmond County and we serve that population because at least three or four perinatal units were forced to close in rural areas of our health district,” Ray said. “As soon as a perinatal center closes, you lose your pediatricians in that area and you certainly lose your obstetrician/gynecologists because if you can’t deliver a baby in an area, you’re not going to stay.”
Ray, who is also the director of the Global Health Program in Obstetrics and Gynecology, helped develop the Georgia Center for Obstetrics Re-entry Program a few years ago. Georgia CORP is one of only a handful of programs that provides a path for obstetricians to become recredentialed and come back to the practice, he said.
In addition, the state is looking for ways to help low-income mothers continue to receive care after giving birth. Just last year, the Georgia General Assembly and Gov. Brian Kemp signed into law House Bill 1114, which extends Medicaid for low-income mothers from two to six months postpartum, Ray said.
“While we would have loved for them to extend Medicaid to a year, we also realize this past year, we had a global pandemic and money is tight,” Ray said. “So, we were happy to be able to get passed an extension for maternity care as it relates to Medicaid. Now, we can cover women in that first six months in the postpartum period, which I think is a great first step.
“It has the potential to have a huge impact on maternal mortality and certainly severe morbidity, which is a much more common problem.”
Dr. Freddy Montero, a maternal-fetal medicine specialist at Augusta University, said ensuring that patients can receive Medicaid coverage six months after their pregnancy will save lives.
“Dr. Ray has really been lobbying the state and even lobbying at a national level for increased health care coverage for our patients,” Montero said. “He’s making sure that our patients’ voices are heard and, as a result, we’re able to not have limitations or challenges when it comes to Medicaid coverage for patients. It’s incredible.”
Augusta University also has a few doctors and a midwife who regularly visit rural areas of the state, such as Jefferson County, to help patients who can’t always make the drive to Augusta, Montero said.
“A lot of what we do here in our practice as a maternal-fetal medicine service is counseling patients and making sure that they understand the importance of adhering to a diabetic diet and what that actually means, and how to check blood sugars and how to administer insulin,” Montero said. “We empower these patients, especially those patients who don’t live nearby. We help them be more independent and self-reliant.
“We’ve also talked to some of the health care providers about setting up satellite offices or satellite stations in their practices. That way, instead of having a patient drive all the way here to Augusta, we can set up telehealth appointments and counseling sessions with those patients.”
Later this year, Obstetrics and Gynecology is also planning on teaming up with the Division of Cardiology at Augusta University to establish a program to address some of the health issues facing women before they get pregnant, Ray said.
“We know that African American women have more cardiovascular disease and, unfortunately, when there’s less access to care, we’re also more likely to see poor health when women are entering pregnancy,” Ray said. “So, one of our initiatives here at Augusta University is a partnership between obstetrics and cardiology to develop a cardio obstetrics program that will focus on maternal mortality and severe morbidity.”
The goal is for the collaborative team to reach out and treat women of reproductive age by working with primary care partners in the region, he said.
“We want to encourage these women to see an obstetrician/gynecologist or a maternal-fetal medicine specialist and provide preconception counseling,” Ray said. “Then, we want to offer to get them in the cardio obstetrics program, where they would see cardiology and have optimized care for their hypertension and diabetes. So, when they enter pregnancy, they would be much healthier.
“It’s really an initiative for us to impact women before pregnancy, but also during and after pregnancy.”
A key to the success of this program will be the nurse navigator, Ray said.
“A nurse navigator would coordinate the care between the multiple services and specialists that would need to be involved,” Ray said, adding he is working with the Department of Public Health to establish the position. “It looks very promising and I think this is a program that will be really unique to the entire state of Georgia.”
When pregnant or postpartum women have to drive more than an hour to see an obstetrician because they live in rural areas in Georgia, distance can become a huge barrier to receiving proper health care.
Dr. Marlo Vernon, an assistant professor in Cancer Control, Prevention, and Population Health in the Georgia Cancer Center, is determined to help make health care easier for mothers across the state. She is developing a new pregnancy care app to give health care providers a better way of monitoring their patients remotely.
The Vida Rural Postpartum and Pregnancy Monitoring (RPM) app is being developed by Vernon to provide doctors with real-time patient data, including sudden changes in blood pressure, rapid weight gain and self-reported mental health updates.
This new app was selected as an awardee in the first and second phases of the Remote Pregnancy Monitoring Grand Challenge, an innovative technology-based competition conducted by the Health Resources and Services Administration (HRSA) Maternal and Child Health Bureau.
Vernon received $35,000 to continue developing her app and will present her final findings in the last phase of the challenge at the end of April. If her prototype is selected, she could receive up to $150,000 and have her app tested on a larger scale, she said.
This app was created to save women’s lives. It was inspired by a loved one whose life sadly wasn’t able to be saved, Vernon said.
“I lost my cousin. She was 38 weeks pregnant,” Vernon said. “She woke up after her baby shower with a terrible headache that wouldn’t go away, which is a classic symptom of developing preeclampsia. By the time she got to the hospital, it was too late.
“They were able to save her baby and he’s now 3, but they weren’t able to save her. So having that history in our family, it really inspired me to look for a simple solution to help women.”
As a result, Vernon developed this pregnancy monitoring system so women could easily self-report medical information to their providers.
“With this app, which people can access on their computer, women take their blood pressure daily and if it reaches above the threshold for what’s considered normal, they receive follow-up questions asking about a headache,” Vernon said. “They are asked if they feel nauseous, if they’re unusually swollen, if they have pain in their stomach or in their chest area. Those are all symptoms of what may be preeclampsia developing.”
The women are then directed to contact their health care provider if they are experiencing any of those symptoms, Vernon said.
“We also have them track their weight once a week, because rapid weight gain could be a symptom of water retention, which could be a symptom of developing hypertensive disorders,” she explained. “And we ask about their mental health because a lot of women don’t know that they can develop postpartum depression up to one year after birth.”
Vernon is hoping this app can help significantly reduce Georgia’s maternal mortality rate in the future.
“The recommendation is to have your first prenatal visit in your first trimester, but for women who don’t have access to an OB-GYN or a midwife or a doctor who provides that type of care, it’s a real issue,” Vernon said. “Over half of the counties in the state of Georgia do not have a practicing OB-GYN, and if you’re in a rural area and you have to travel to Augusta, for instance, to get your prenatal care, that’s not easy.”
Making such appointments can be expensive, time-consuming and a hassle, Vernon said.
“Not only do you have to take time off from work, you have to have transportation, you have to find someone to watch your other children and you have to wait at the doctor’s office for an extended period of time,” she said. “A lot of women just don’t have the freedom to do that, so they don’t make their appointments within the recommended time and, of course, that contributes to missing developing problems in their pregnancies. The truth is, women who start prenatal care later tend to have worse outcomes.”
There are currently 30 women in Georgia volunteering to test Vernon’s app, she said.
“We have 15 women in south rural Georgia and 15 in our area using the app,” Vernon said. “We found that, overwhelmingly, women want to have some understanding of what was going on with their health. This app gives them some of those tools to know what’s normal, what’s not and what to do if they or someone they know start experiencing any of these symptoms.
“Women just want to be empowered and this app will help them.”

From 2008 to 2017, 9,707 Georgia infants died before their first birthday, according to the Georgia Department of Public Health. That’s a terrible reality that the state is trying to change.
Infant mortality is defined as the number of deaths occurring in the first year of life per 1,000 births, according to the World Health Organization. In 2017, Georgia’s infant mortality rate was 7.2 deaths per 1,000 live births.
Between 2013 and 2017, more than half of infant deaths occurred within the first six days of life and prematurity was the leading cause of infant deaths in Georgia.
Similar to the maternal mortality rate in Georgia, the infant mortality rate among Black infants was two times higher than white infants. About 12.2 Black infants die per 1,000 live births compared to about 5.4 white infants.
“Black infants have about twice the mortality of white infants and that’s actually been the case for more than 100 years now,” said Dr. Paul Mann, chief of the Division of Neonatology and associate professor of pediatrics at Augusta University. “If you go back to 1850, Black infant mortality was about 1.6 times that of white infants. So, the disparity has actually gotten worse with time, even as the overall infant mortality rates have gone down.”
Mann is currently writing a book chapter exploring unique contributors to infant mortality and outcome disparities in Georgia and the South.
“The chapter discusses, in part, how our state fares compared to other states and the factors that make us more vulnerable to higher infant mortality rates,” Mann said. “It also discusses opportunities that we have to improve that situation.”
Mann outlines the history of infant mortality and the fact that, overall, the country’s rate has come down.
“A lot of that is overcoming poverty and disease that were large historical drivers of infant mortality,” Mann said. “But the tragic part of the story is, while U.S. infant mortality overall has improved, we’ve yet to close the gap for our Black infants. And I’m trying to explore questions such as: How does the neonatal intensive care unit (NICU) environment impact those outcomes? How do we optimize infant safety once home? What are the community-level factors that will help reduce the accidental deaths and sudden infant death syndrome? And what are the systemic factors that contribute to outcome disparity?”
Mann explained there are several factors that contribute to Black infants being more vulnerable to infant mortality.
“The top five reasons that Black infants have more infant mortality are premature birth or low birth weight followed by congenital malformations, maternal complications with pregnancy, accidental injury and sudden infant death syndrome,” Mann said. “The biggest contributor, however, is premature birth. If we were to reduce premature birth rates for Black mothers, we would reduce about 50% of the infant mortality disparity that’s seen between the Black and white populations.”
For all babies in Georgia, prematurity, respiratory conditions and cardiovascular disorders, along with sudden infant death syndrome, are the most common causes of infant mortality in early, late and post-neonatal infancy periods, according to the Georgia Department of Public Health.
“From a public health standpoint, we have a long way to go to reduce other drivers that lead to these mortality disparities, from food and housing insecurity to community access,” Mann said. “We know that infants, both Black and white, who live in rural communities are more likely to have infant mortality than urban communities and a lot of that deals with issues related to health access.
“One of the big concerns that I have is, we’re in the midst of this COVID pandemic and rural hospitals are suffering. Many have closed and many more will close.”
The further closures of rural hospitals will inevitably impact the health of both mothers and babies, Mann said.
“About 10% of Black moms receive late prenatal care when they’re pregnant. That’s at least more than twice the rates of white women,” he said. “Therefore, we have a long way to go to providing a healthy pregnancy for Black women that would, at least, begin to impact the issues of premature birth and low-birth weights.”
Several studies over the years have indicated more positive outcomes for African American mothers and infants who are cared for by Black physicians, Mann said.
“We see that Black mothers have better outcomes when there are black caregivers that are providing them support during their pregnancy,” Mann said. “One of the things that had been suggested, and that some communities have done, is to support Black mothers with Black doulas to help them better navigate the pregnancy process and to optimize their medical care.”
A doula is a person trained to advise, inform and offer emotional and physical comfort to a mother before, during and after the birth of her child.
“So, certainly one of the first things that we need to do is to diversify our workforce, in order to provide that support,” Mann said. “And I think that the Medical College of Georgia has done a good job working to diversify its student body. And, from specialty to specialty, we have to look at how are we doing in creating an inclusive environment? And once the students choose our specialty, do we have a culture that retains and values differences?”
The Society for Maternal-Fetal Medicine has found that Black patients are 2.94 times more likely to report they’ve had all of their medical needs met if they are treated by a Black physician, Montero said.
“African American patients with Black physicians are also 1.74 times more likely to report receiving preventative care compared to those with other physicians,” Montero said. “So, I think a patient having a doctor that they can relate to on a much larger scale and a different level, other than just, ‘I’m here for health care,’ really makes a difference.”
As an African American physician, Bullard said she sees firsthand the positive impact a diversified staff can have on patient care.
“I knew from a young age, probably since I was 12, that I wanted to go into medicine,” Bullard said. “But why I stayed interested in medicine was because I saw the enormous benefits.
“I love just advancing women and I know my little bit of work goes a long way in impacting someone’s life.”
Statistics show there is a disproportionate impact of HIV on racial and ethnic minorities. It is estimated that Black men will lose their lives to AIDS at six times the rate of white men, according to the Centers for Disease Control and Prevention. The Ryan White Program at the Medical College of Georgia is working to improve the health of these patients while also preventing new cases in the community. Next in this series, we’ll take a look at the issue and the progress being made.

