As of 2023, there were 4,606 total physicians specializing in managing pulmonary diseases in the United States. That is 128 fewer than the previous year, which adds to the overall trend of a growing physician shortage, according to a report by the Association of American Medical Colleges.
For seven years now, the Medical College of Georgia at Augusta University has served as a training hub for pulmonary procedures, welcoming fellows from medical colleges across the Southeast in efforts to bridge the gap between workforce and care.
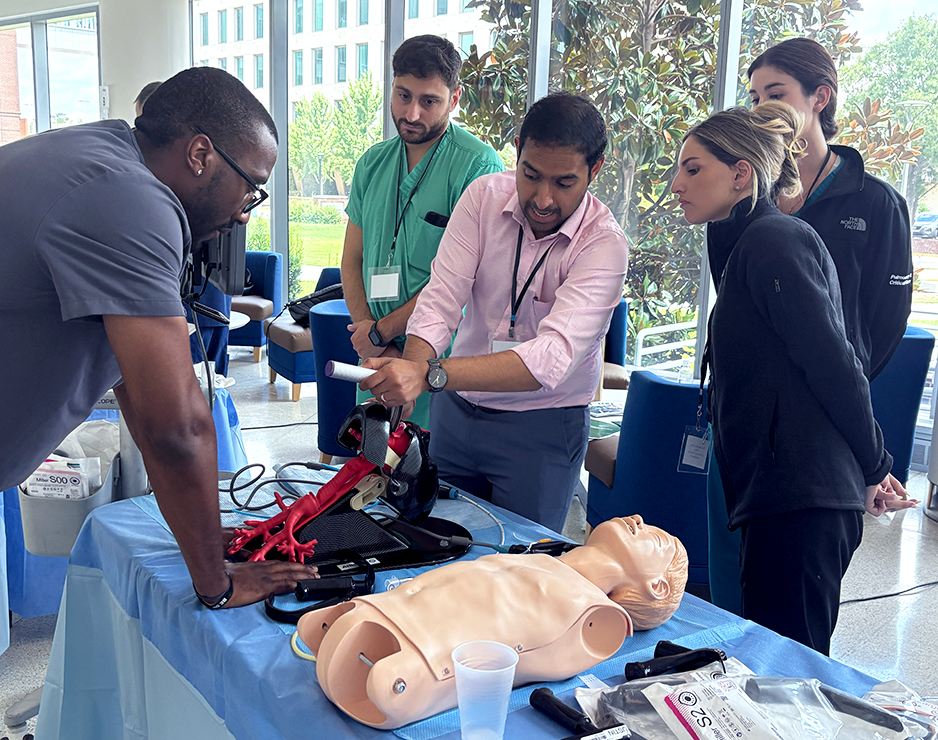
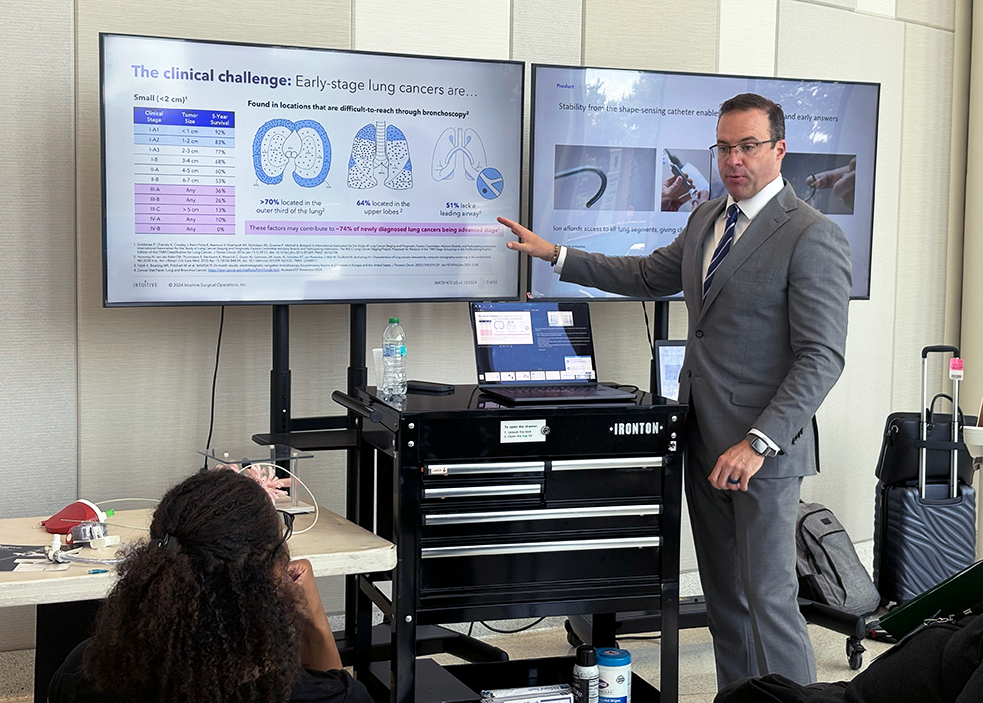
A main component of that is utilizing new technologies and robotics in the pulmonology field, which have allowed procedures to become more specialized to serve each individual case. The main goal of the training is to introduce fellows to these advanced tools and techniques in order to elevate their expertise.
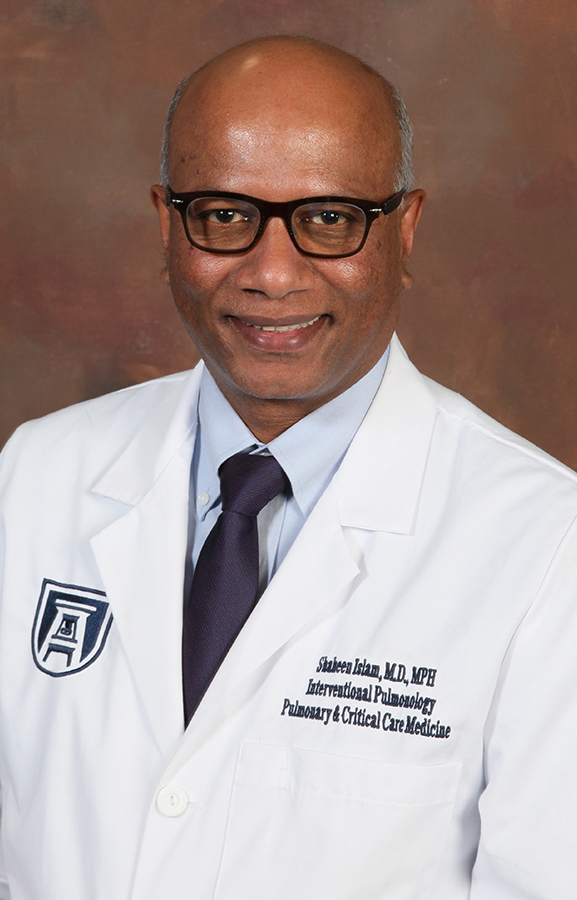
“When I was a fellow and I did my training years ago, we were just told to see the patient, do the procedures and then teach it. See one, do one, teach one,” said Shaheen Islam, MD, professor of medicine and division chair and director of Interventional Pulmonology at MCG. “But the problem is those are difficult procedures. When I became an attending physician, my whole idea was to give new fellows training away from the patients in a simulated environment – they can practice as long as they want, so they’re ready to take care of those patients.”
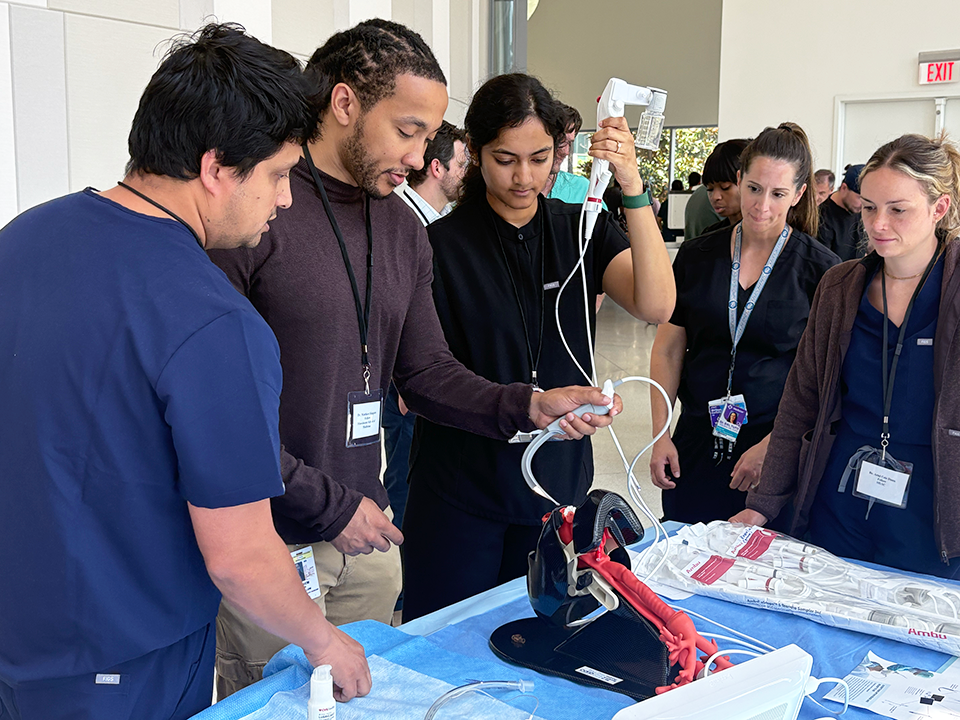
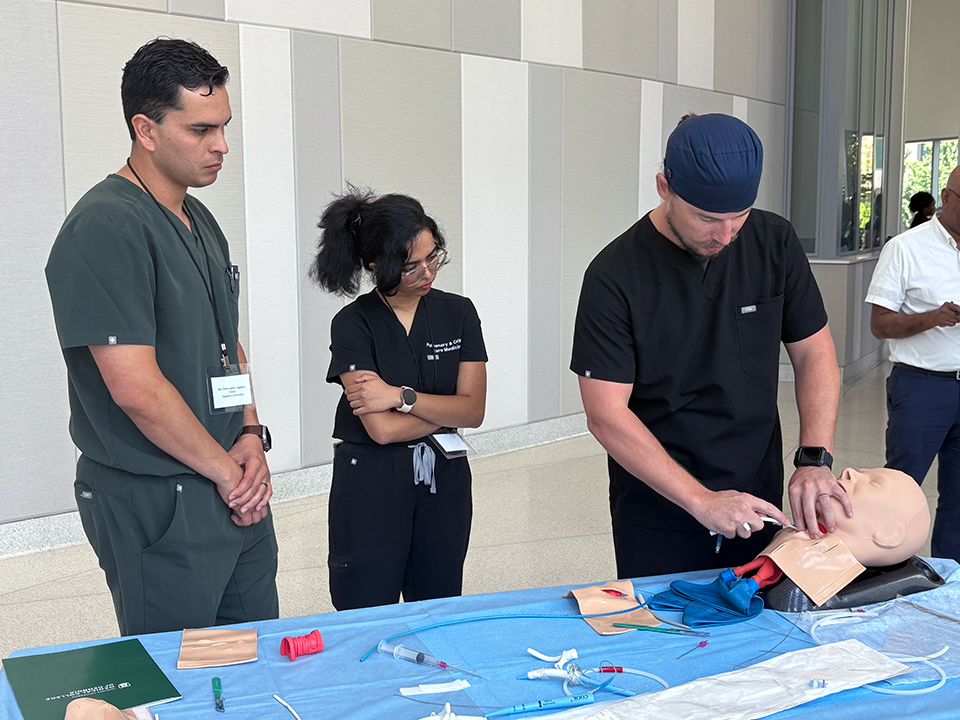
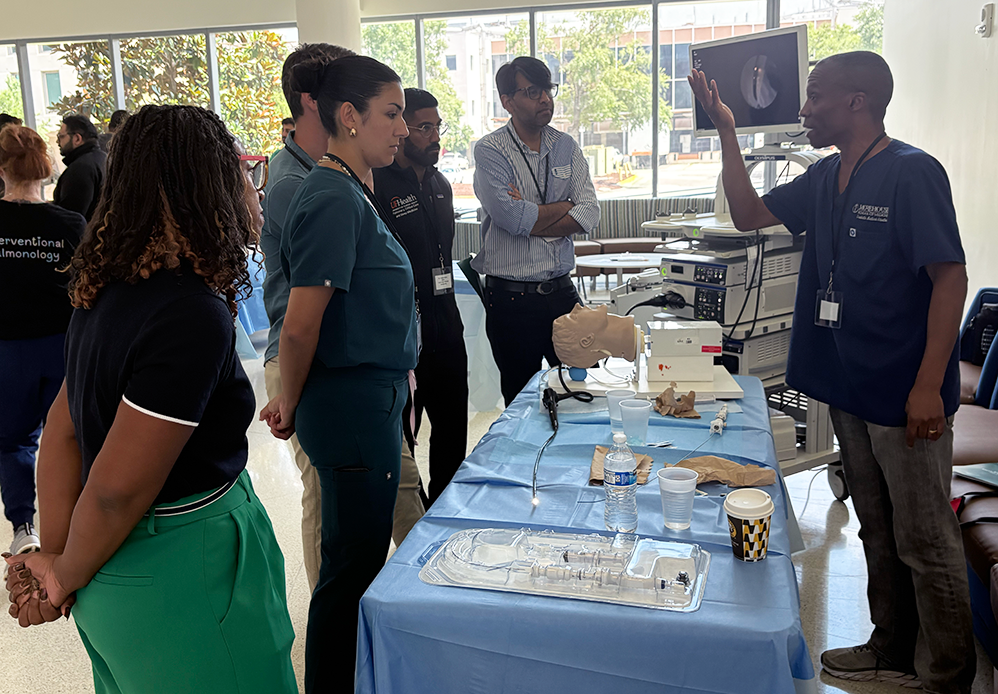
Earlier this semester, close to 40 fellows from MCG, the Medical University of South Carolina, the University of South Carolina School of Medicine Greenville and Columbia, the University of Florida Jacksonville, Emory University School of Medicine and Morehouse School of Medicine gathered at the J. Harold Harrison, MD Education Commons and the animal and cadaver labs to learn and practice pulmonary techniques at 10 hands-on training stations.

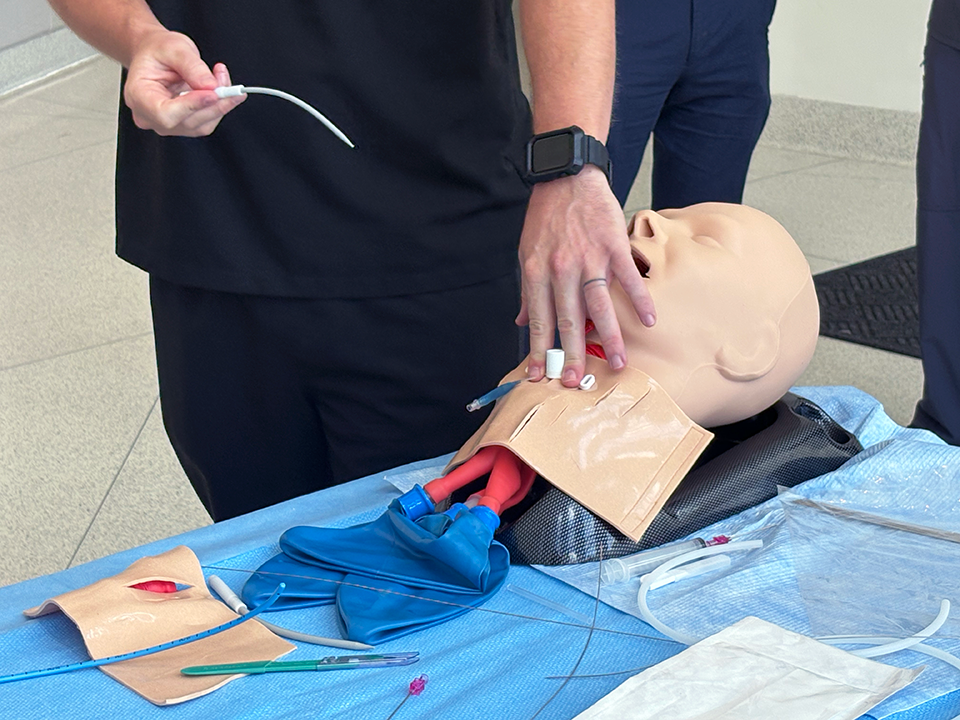
In addition to learning common pulmonary procedures, the fellows learned how to remove foreign objects from airways, diagnose infections in the lungs, manage difficult airways and place and manage chest tubes.
“It’s very eye-opening – there are so many new non-invasive ways to do different biopsies or techniques,” said Christopher Aguirre, DO, a pulmonary critical care medicine fellow at MCG. “It’s a very great course early on in our fellowship to get an overview of every type of procedure and every type of device, because here’s like 10 of everything to get familiar with and to get used to using before you’re out there practicing in the real world.”
One of those new techniques is a robotic bronchoscopy, which was Aguirre’s favorite training station.
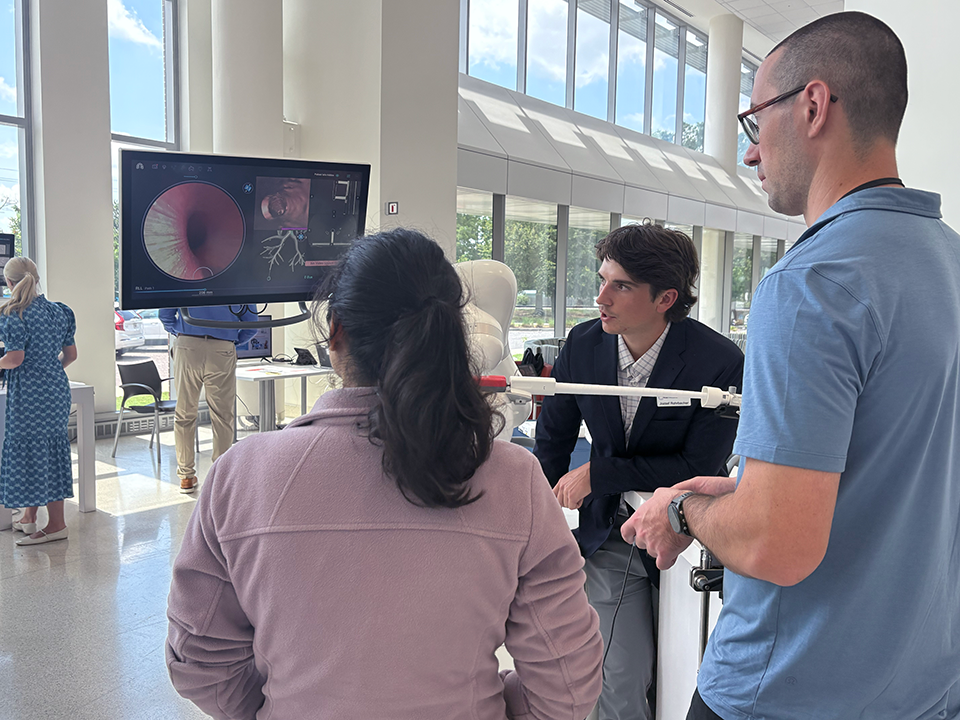
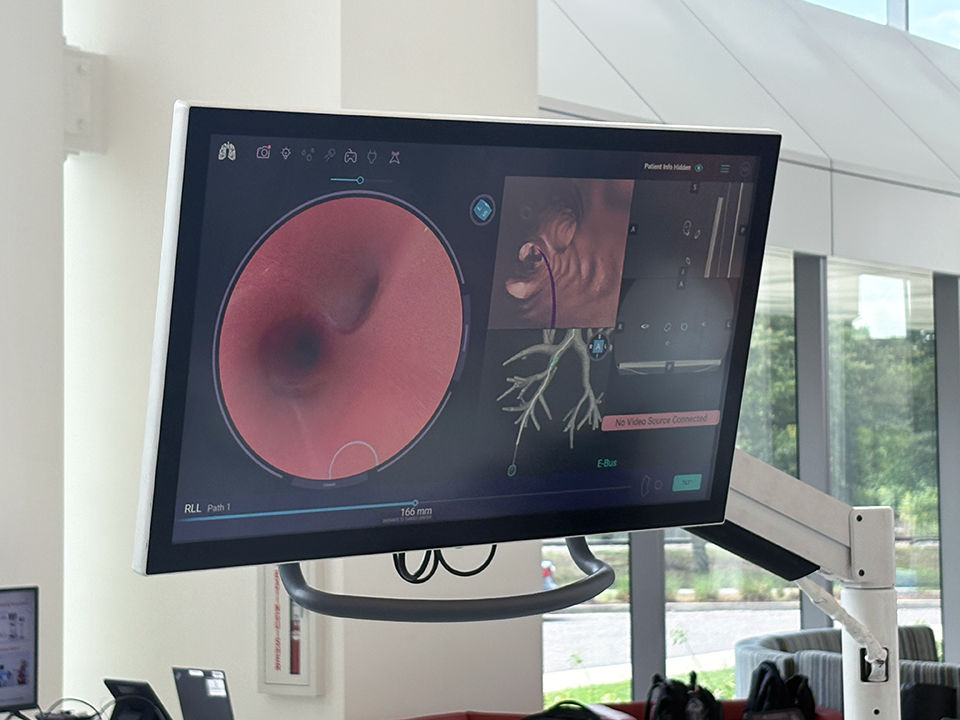
“It feels like I’m playing video games again. It’s a really cool device, and it’s going to be used more widely because it’s so noninvasive. The old way was doing a CT-guided biopsy coming from the outside of the body – now we can use this robotic bronchoscopy and reach the outer portions of the lungs that used to be impossible to get to,” he said.
Aguirre, along with the other fellows, started their fellowship programs on July 1, and they will take about three years to complete and receive board certifications. Attending this “boot camp” training of sorts with other fellows from the Southeast is not only an opportunity for them to grow and develop their skills but also to network with their professional peers.
“Occasionally, there will be research projects that fellowships will do with other fellows. Like the University of South Carolina in Greenville will have a research project, and they’ll ask us to see if our patient population matches their research project,” Aguirre said. “And today, some of the new program directors and some of the faculty at other programs have different ways of doing things that you pick up, and you’re like, ‘Oh wow, I never knew I could do it this way.’ There are a lot of different techniques out there, and everyone gets to learn something new, and you get different tools in your toolbox that you can use later on.”
Faculty members from the different medical schools served as instructors.
Steven Allen, MD, an interventional pulmonologist at MCG, was an instructor at the thoracic ultrasound station and the chest tube station. He said many of the schools represented at the training don’t offer the specific pulmonary courses that MCG does, so it showcased the level of expertise the college has, especially with emerging pulmonary techniques.
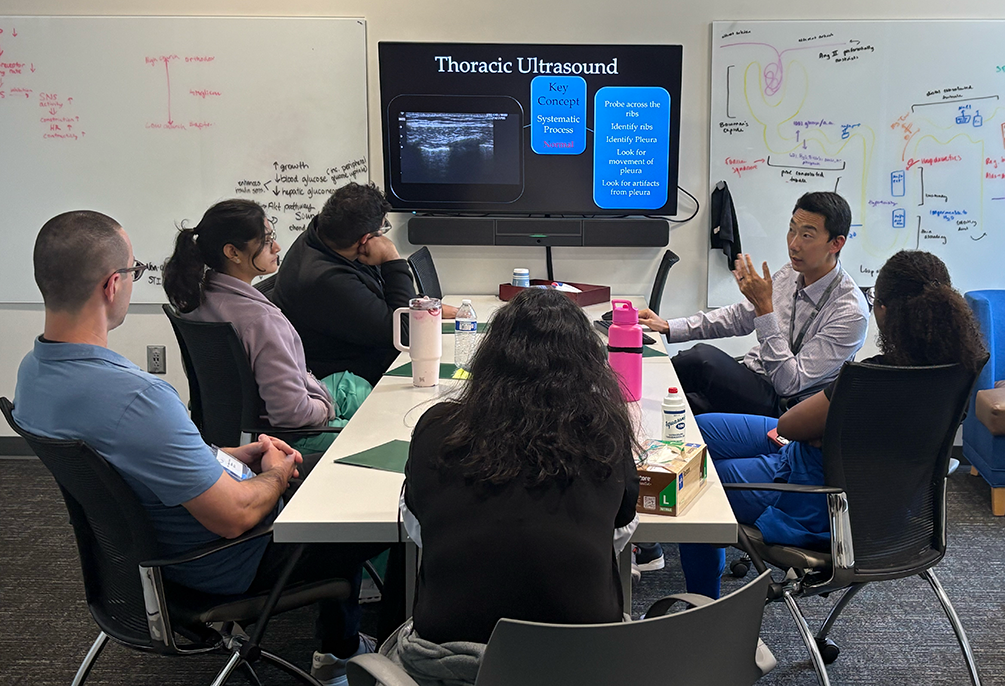
“We actually do a feedback session for all the fellows, and for the most part, everybody says it’s a good experience. Going into it, a lot of them think it’s going to be super basic with a couple of lectures, but then they are quite surprised when they get good hands-on experience,” he said.
Aside from advanced technologies, the leadership team is introducing the trainees to more simulated exercises.
“We were in the cadaver lab, and that’s been a long-standing practice to practice these techniques on animal or human cadavers, but we now have a lot of high-fidelity simulations that we can do outside of that, where they’re able to replicate some of those procedures in a way that we can observe them do it, give them feedback and prepare them for doing it in real life,” said George Carter, MD, a pulmonologist at MUSC.


Islam, the course director of the event, said half of the fellows will usually stay in the region after they complete the fellowship, which will allow for more patients to be sent to MCG for treatment. He hopes to continue hosting this training in the future and to expand it more each year.
“One, we’re giving them a more diverse opportunity to learn. And two, I think this also creates a reputation for MCG in the Southeast region, and all those programs are continuing to send their fellows here,” he said.
 Augusta University
Augusta University




