When someone says the word “hospice,” words like “illness” or “dying” might come to mind. But for Ashley Perkins, it’s more than that.
“We bring life to the rest of the time you have. It’s about what’s important to you, and how we can help you with that,” Perkins said.
Perkins is graduating from the Doctor of Nursing Practice Nurse Executive program through Augusta University’s College of Nursing. The program is designed exclusively for chief nursing officers, vice presidents of nursing and other nursing leaders aspiring to pursue executive-level nursing positions.
Already a vice president of hospice services at a not-for-profit organization, Perkins pursued an advanced degree to be able to contribute more.
“I just became consumed with the idea of furthering my education,” she said. “I felt like I reached a point in my career where I could do more, take my leadership further and effect more change.”
Many leaders in health care have backgrounds in business, which Perkins maintains is an important piece of a successful system. But she also believes those who have been at the bedside should be the ones making decisions that affect patients.
“Nurses belong at the table. When you look at quality, outcomes, satisfaction – all of those require nurses,” Perkins said.
Perkins’ goal is to utilize her strategic thinking to advance health care and be part of the bigger picture. Now armed with the knowledge from her education, she feels she can be more active in executive meetings and more confident in her abilities to contribute.

Leadership has been a focal point throughout her nursing journey. Starting at just 16 years old as a certified nursing assistant, those leaders who guided her played an influential role in her goals. She eventually received her Master of Nursing in Leadership and Management from Western Governors University.
“I love helping others and answering questions,” she said. “Making other people think outside the box, it leads to innovation and improvements to what we are doing. There’s always something new and a question you’ve never been asked, but your experience helps you to figure it out.”
Along with a passion for leadership, Perkins has been a hospice nurse for the last 15 years. When her grandmother needed hospice services, Perkins was inspired by how big of an impact the nurses had on her entire family. She knew immediately that’s where she wanted to be.
“As a hospice nurse, there’s no hurry. I’m with you right now; you’re the world right now,” Perkins said. “We get to really connect with these people and will forever be a part in their story. We can make this sad time in their lives better, and that’s amazing to me.”
Perkins wants others to understand that hospice care is about choosing what is best for the patient’s situation. They are in control, choosing to be comfortable and happy in the best way they can.
“There are many misconceptions about it, and I’d love for others to understand it more,” she shared. “Every person, regardless of background, status or diagnosis, deserves comfort and dignity at the end of their life. We help you live well through the end of your life, whatever that means to you.”
Much of Perkins’ work extends beyond the patient. Her team helps families navigate the entire process. Hospice nurses continue to provide resources, such as bereavement support, even after the patient has passed.

As a DNP student, Perkins was required to complete a capstone project in an area of her expertise. She combined her passions for hospice and research, focusing on how to be more proactive for patients with chronic illnesses like heart failure.
“I thought about those we serve and how we can better anticipate their needs,” she said.
In hospice, patients are served wherever they choose to reside, which could be their own homes, assisted living facilities or on the in-patient unit. Perkins developed two kits to better assist patient care, wherever they are.
“We developed a medication kit and a tool kit. The tool kit helps them to keep track of their vitals while the medication kit provides symptom management,” Perkins said.
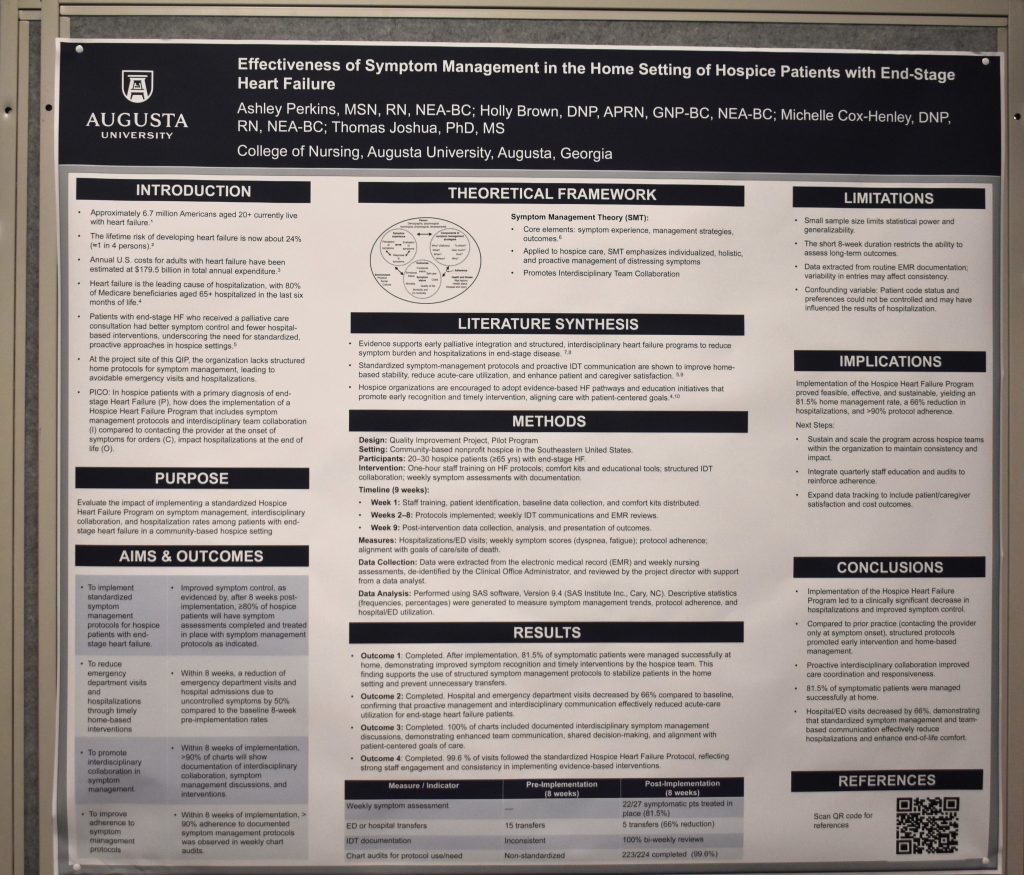
The tool kit includes items like a blood pressure cuff, scale and an oxygen stat machine. The medication kit has tailored medicines, such as a diuretic to take in the result of weight increase and breathing problems.
“We have decreased hospitalizations and improved symptom management in the home,” Perkins said. “It’s been so beneficial for our patients with end-stage heart failure, and we are excited to expand it out to the rest of our patients.”
For Perkins, this type of work is the exact reason she wanted to pursue her doctorate with AU’s College of Nursing. Earning her advanced degree has further solidified her passion and experience, positioning her to make a lasting impact in hospice care and the lives of her future patients.
 Augusta University
Augusta University