There appears to be an unhealthy synergy between mental illness and prostate cancer, and researchers are working to dissect the relationship by first assembling the largest dataset ever of veterans with either condition or both.
Prostate cancer is the most common cancer diagnosed in the massive Veterans Health Administration network that sees about 9 million veterans annually who today are about 90% male.
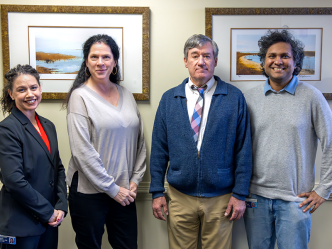
“It’s the largest and most connected health care system we have that can provide the sample size and follow up data to enable this large-scale assessment,” says Dr. Zachary Klaassen, urologic oncologist in the Department of Surgery at the Medical College of Georgia at Augusta University.
Klaassen, director of clinical urological research at MCG and the Georgia Cancer Center, just received a $750,000 grant from the U.S. Department of Defense that is enabling investigators to scour the massive datasets of the VA since 2000 for men with mental health illness, those with prostate cancer and those with both so they can compare conditions and outcomes. He expects 20 or more separate research projects will ultimately come out of this new database over at least the next decade.
“We think there may be a correlation between mental health and aggressiveness of prostate cancer and we think patients who don’t get mental health care may not be getting the same treatment and follow up for their prostate cancer,” he says.
“So we want to see the impact of mental health on when you are diagnosed, how old you are, how aggressive the cancer is, compared to people who don’t have mental illness,” Klaassen says of the database he will develop over the next several years.
One working hypothesis is that if you have a mental illness like depression, which is pervasive in society and known to be even more common in patients with cancer, you may pay less attention to your body and overall health, and may be less likely to get screened for prostate cancer and/or seek help, says Klaassen.
“They may not have the capacity or social support to make or get to an appointment,” he says, which can mean diagnosis is delayed and the cancer is more advanced when it’s found.
There likely also are biological risks with factors like inflammation, which is increased in both cancer and depression, that might make the cancer more aggressive, says Klaassen, who also wants to look at inflammation markers in these patients.
One of their first explorations of the massive dataset will be to determine whether having a mental health illness diagnosed prior to their prostate cancer diagnosis impacts the treatment received, patient’s adherence to the planned prostate cancer treatment and follow up, and cancer outcomes.
They think that while having both conditions may worsen prostate cancer outcomes, getting treatment for mental illness at the VA may equalize cancer outcomes for patients with and without mental illness.
If they are correct that getting good mental health care, including things like therapy sessions and medication, means better cancer outcomes, it would definitely be a win for patients and the VA health system, which is known for excellent programs helping address the mental health problems of veterans, Klaassen says.
“If we find they are not the same then we have actionable items to figure out why not,” Klaassen says, possibly like better prostate cancer screening in men with mental health problems and mental health assessment in patients with prostate cancer.
Klaassen, a native of Canada, who completed his urologic oncology fellowship at the University of Toronto and Princess Margaret Cancer Centre after a urology residency at MCG and AU Health System, has extensively studied the intersection of mental illness and prostate and other cancers in Canada. He is among many investigators to see patterns of more mental health problems in patients with cancer and worse cancer outcomes in patients with mental illness.
“If you look hard enough, you likely will find a proportion of our patients are clinically depressed even before their prostate cancer diagnosis,” says Klaassen, the Ronald W. Lewis, MD Endowed Chair for Urologic Education, of the often successful but arduous task of battling prostate cancer.
Even with advanced disease, many men may live for several years while others may die of other causes rather than prostate cancer.
“Prostate cancer may not kill you but life with it can be very difficult,” Klaassen says. “Patients get all this treatment, they may get side effects like erectile dysfunction and urinary incontinence from their treatment, and advanced treatment like hormone therapy, is known to cause problems like depression, dementia, bone and muscle loss,” Klaassen says.
In 2017 in the journal Urologic Oncology, Klaassen and his colleagues reported that men with prostate cancer most at risk for suicide were white, unmarried males with metastatic disease and that about 60% of men with prostate cancer also have mental health distress— 10-40% with clinically significant depression. That depression risk increases with hormone therapy, a common treatment in the advanced stage of this male hormone-driven cancer. Investigators then recommended screening for erectile dysfunction, depression and suicidal thoughts in patients with prostate cancer as a standard part of treatment.
Klaassen and his colleagues reported earlier this year in the journal Cancer, after looking at 676,470 Canadians with cancer and 2.2 million without, that a cancer diagnosis is associated with an increased risk of death from suicide even if the patients with cancer had psychiatric care before their cancer diagnosis. Others including Klaassen have helped show that about 70% of suicides in people over age 60 are associated with a medical illness, and rates are even higher in those with cancer.
Also earlier this year, Klaassen and his colleagues reported in the British Journal of Cancer in that same large group of patients with cancers, including common malignancies like prostate, breast, lung and bladder cancers, that those with psychiatric problems before their cancer diagnosis had both worse cancer-specific mortality and all causes of mortality.
While factors underlying the association remain unclear, they theorized that those seeking psychiatric help before the diagnosis would be more “at risk” and have poorer survival. Those admitted to a psychiatric facility and later diagnosed with bladder or colorectal cancer were particularly at risk for cancer-related death compared to those without a psychiatric history.
While the whys of these associations are unclear, it may be, for example, cancers like breast and prostate cancer, which are associated with sexual well being, may be particularly difficult for patients who have already had to seek psychiatric help, they wrote. Other investigators have had similar findings and theories.
Last year, in European Urology, Klaassen and others reported an uptick in the use of antidepressants following surgery or radiation therapy for nonmetastatic prostate cancer but not in those who simply were kept under close watch, an option when the cancer is low grade and slow-growing. Their finding underscored the need for also providing psychological support to patients, they reported.
Major depression is one of the most common mental health disorders in the United States, according to the National Institute of Mental Health, with about 7% of all adults experiencing as least one major depressive episode.
The prostate is a walnut-sized gland between the bladder and penis that secretes supportive fluid for the sperm. Prostate cancer occurs in 1 out of 9 men over their lifetime, is the most common cancer in men in the United States, other than skin cancer, and the second leading cause of cancer death in men, behind lung cancer, according to the American Cancer Society. Risk factors include aging, obesity, smoking and chemical exposures like Agent Orange, as well as inflammation of the prostate.
 Augusta University
Augusta University