Dr. Richard A. McIndoe, bioinformatics expert and associate director of the Center for Biotechnology and Genomic Medicine at the Medical College of Georgia, is leading a dynamic new $6.2 million federally funded initiative to support highly innovative research ideas in three areas with tremendous impact on health.
This Innovative Science Accelerator, or ISAC, program establishes an expedited but still extensive review process that will enable scientists to pursue some of their most innovative research ideas in diseases of the kidneys; the urinary tract in both sexes as well as the male reproductive organs; and the blood and bone marrow.
“The idea is that ISAC will provide seed funds to investigators who have high-risk, high-reward ideas, and they will get one year of money to try to figure out if their idea is going to work. If it works, they will be able to use the data they generate to apply for a larger grant,” says McIndoe, who wants the new program to be as innovative as the ideas scientists bring to it.
The five-year initiative is a new program of the Division of Kidney, Urologic and Hematologic Diseases of the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health.
The goal is to move science forward that matters to people’s lives, and the opportunities include giving particularly new scientists experience writing grants, going through the review process and generating findings, McIndoe says.
ISAC will provide scientists an efficient path to secure a one-time $100,000 grant that should ease application for a larger, traditional NIH grant, the gold standard for biomedical research in the U.S., or conversely to acknowledge that their idea does not merit additional pursuit.
Another primary function of ISAC is to host an annual scientific meeting for scientists working in these areas where awardees can present their work, and that will help fuel discussion and collaboration, says McIndoe, Regents’ Professor and Georgia Research Alliance Distinguished Investigator.
High-risk research with high-reward potential often doesn’t get funded in the traditional, highly competitive process of seeking NIH funding, McIndoe says. For example, the 2019 payline for the NIDDK was 13%, which means only 13 of 100 submitted grants get funded.
About half of submitted grants, don’t even make it through the NIH study section manned by experts in the field who do the frontline review of grant proposals, says McIndoe, who at points in his career has sat on more than a half-dozen study sections annually.
As director of ISAC’s coordinating unit, McIndoe will also work with NIH program officers with expertise in the area of interest of an application to identify other experts across the country. He’ll then manage the review process from there, including assigning reviewers and making sure reviews are done on time.
He’ll ensure that the scores and critiques get back to the NIH program officers who also will rank the grant proposals, and that information along with what the ISAC office determines to be a fundable score range will then go to one more group of experts in the field, ISAC’s External Evaluation Committee, and if they agree with the determinations, the decision is made.
Although the review process is extensive, it’s about half of the standard process for submitting for scientists and reviewers alike, starting with a three-page research plan rather than up to a dozen pages for an RO1, the NIH’s oldest grant mechanism, and the application is easier for reviewers to digest, McIndoe says.
The ISAC Working Group recently opted to have three application review times annually to further expedite the process, and applications can be submitted at any time, McIndoe says. Scientists can begin submitting applications this fall, and the first annual meeting likely will be next Spring.
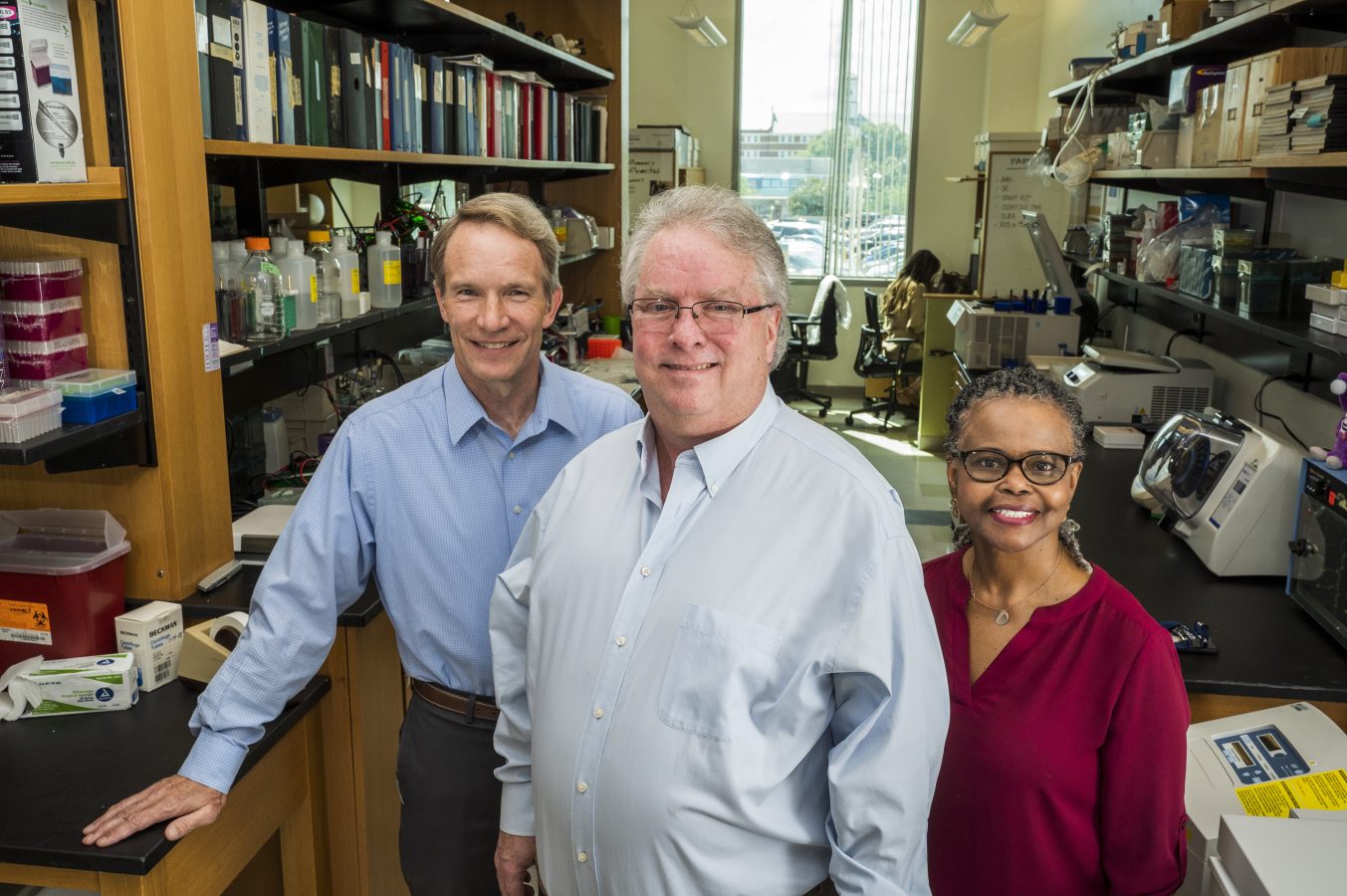
The local ISAC Working Group, which will advise McIndoe on kidney, urologic and hematology research, includes Dr. David Mattson, chair of the MCG Department of Physiology and an established hypertension researcher; Dr. Jennifer Sullivan, pharmacologist and physiologist in the Department of Physiology who is also interim dean of The Graduate School at AU and studies blood pressure regulation and kidney health, with a particular interest in gender differences; and Dr. Betty Pace, pediatric hematologist in the MCG Department of Pediatrics, an established sickle cell physician scientist who leads a federally funded national initiative to inspire the next generation of investigators.
ISAC’s target areas may change annually based on what’s happening in the scientific literature and what experts in respective fields identify as hot topics that need pursuing. The Working Group and the annual meetings will further enable those discussions and decisions.
McIndoe, an expert in managing and analyzing large amounts of data, has already managed two other innovative NIH funding approaches and consequently has a solid infrastructure in place to support this new initiative. For 20 years he has led the Coordinating and Bioinformatics Unit for the Diabetic Complications Consortium to fund shorter-term laboratory and human studies to better understand the complications of diabetes, like heart and kidney disease and vision problems. The consortium began as the Animal Models of Diabetes Complications, which specifically designed and shared good mouse models.
Fifteen years ago he began providing similar services for the Mouse Metabolic Phenotyping Centers, which make the specialized, expensive mouse-testing capabilities of a select number of universities available and affordable to researchers nationwide. Expertise includes things like characterizing mouse metabolism and analyzing blood composition.
Together those NIDDK initiatives, which also hold scientific meetings and support websites to support interested scientific communities, have resulted in thousands of publications that demonstrate new findings and helped scientists secure larger NIH grants. As an example, more than 60% of those receiving a $100,000 grant through the Diabetic Complications Consortium applied for an RO1 and about 25% were successful.
“That’s higher than the normal percentage and a goal of these kinds of programs,” McIndoe says. Both those programs are scheduled to phase out next year.
 Augusta University
Augusta University