Researchers from the Medical College of Georgia at Augusta University were recently featured in an issue of Aging Cell for a study that bridges a noticeable gap in previous literature focused on how obesity can cause chronic inflammation in the female central nervous system.
A common practice in scientific medical studies is using mouse models, but Ali Eroglu, PhD, a professor in MCG’s Department of Neuroscience and Regenerative Medicine, noted most preceding studies use male mice almost exclusively. He noticed far fewer studies used female mice, causing a gap in the understanding of how obesity and possibly other conditions affect females differently than males.
“Previous studies also tended to look at one data point, so it was not very clear how duration of obesity and the age of the subject affected neuroinflammation,” Eroglu said. “Our study was aimed at addressing those gaps.”
Eroglu’s lab is part of a larger team at MCG that has been studying the different aspects of the aging process and the effects aging has on different tissues ranging from bones, skin and muscles to the brain, the central nervous system and everything in between.
Carlos M. Isales, MD, a Regents’ Professor in the Department of Neuroscience and Regenerative Medicine, the J. Harold Harrison Distinguished University Chair in Healthy Aging and chief of the Division of Endocrinology, Diabetes and Metabolism, serves as the clinical director of MCG’s Center for Healthy Aging.
“We are a group that continues to expand as interest around the effects of aging has increased, and we look at different aspects of the aging process, and we come together and discuss what we have found – are there any common mechanisms, whether we are looking at the brain, the bones, muscle or skin tissue,” Isales said. “We are looking for things that are in the aging process that could be a shared target. Some of these issues are so complex that they require groups of investigators working together to address them.”
Obesity is a growing epidemic worldwide. According to a 2024 estimation from the World Health Organization, nearly 2.5 billion adults worldwide were overweight and over 800 million were obese as of 2022. In adults over the age of 18, 43% of men and 44% of women were considered to be overweight.
It’s not something that affects just adults as over 390 million children and adolescents between the ages of 5 and 19 were overweight or obese.
An individual is considered overweight with a body-mass index between 25.0 and 29.9 kg/m2 and obese when a BMI is 30 kg/m2 or higher.
Obesity, which can be caused by reduced physical activity and a high-fat diet, has been linked to severe effects on a person’s aging, leading to low-grade inflammation which, if untreated, could lead to far more serious conditions, including diabetes, heart disease and brain disorders.
Because high-fat foods increase pro-inflammatory cytokines, especially in the hypothalamus, this may lower brain-derived neurotrophic factor levels, leading eventually to neuronal death.
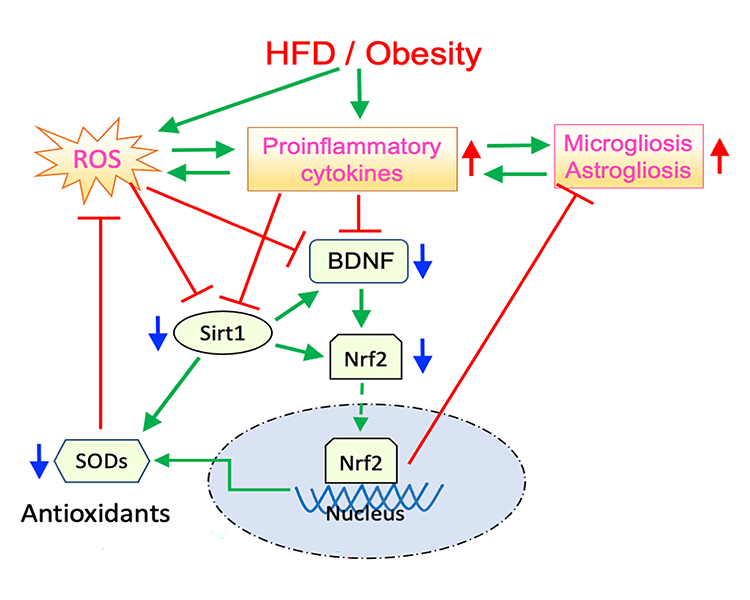
High-fat diets also threaten the neuroprotective benefits of certain molecules, like silent information regulator 1, which stimulates BDNF and antioxidant enzymes.
Mouse studies on high-fat diets have allowed researchers to learn a lot about human obesity, but most only looked at one data point, and did not take age or obesity duration into account. After noticing the gaps around studies on female mice, Eroglu and his team began focusing on studying the effects of obesity duration on brain health, especially in females. The research team included Binnur Eroglu, PhD, a research scientist in the Department of Neuroscience and Regenerative Medicine. She carried out the experiments and contributed to the writing of the manuscript.
“Before this study, I thought the problem began in the fat tissue,” Eroglu said. “The immune cells there release inflammatory cytokines and that induces inflammation in other regions, but our results showed visceral fat tissue inflammation actually starts in the hypothalamus region of the brain earlier than in the visceral fat tissue of young females.”
The research team fed adolescent (5 weeks old) and mature (14 weeks old) female mice a high-fat diet for different durations (13 or 26 weeks) and studied the brain’s inflammation, growth and protection. All mice became obese, but young females showed a mild response in one brain area after 13 weeks. Prolonged obesity led to widespread inflammation and damage. Older females were more vulnerable, even with brief obesity.
The study shows obesity duration is a key risk factor for brain inflammation. Age and obesity duration matter, and early intervention is crucial for brain health.
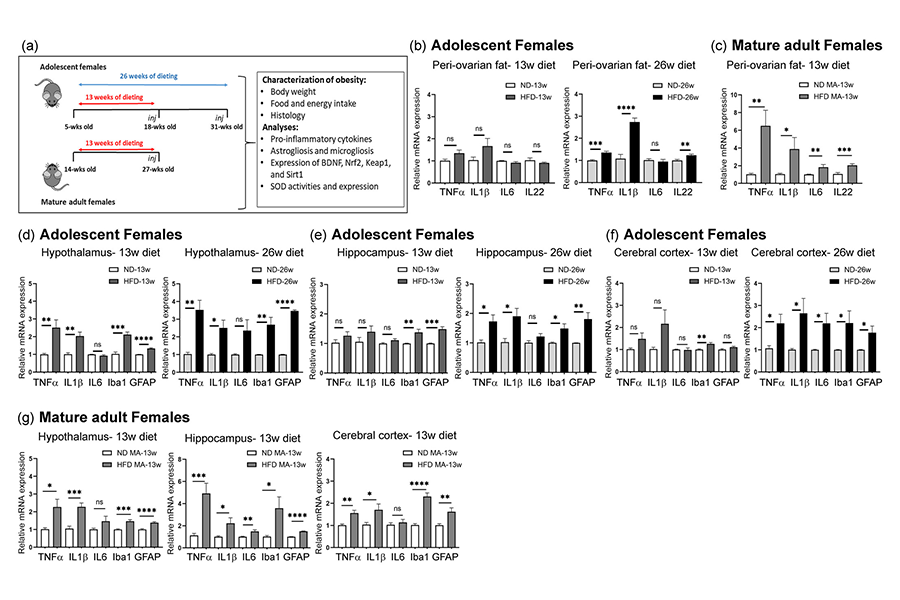
“The results were encouraging because it shows that if you take appropriate corrective measures for younger females who have been overweight or obese, our finding indicates you can avoid brain inflammation without large areas being affected,” Eroglu said. “But the other side of that is if it continues for too long, you may develop neuroinflammation in different brain regions.
“When we looked at mature females, those at a more advanced age, we were able to see the age is also important,” Eroglu continued. “As the female mice age, they became more sensitive to shorter durations of high-fat diet and obesity. Our results are consistent with earlier results, but expand them by showing when you increase the duration of obesity eventually young females also develop neuroinflammation.”
Eroglu noted there are more studies to be conducted around other variables, including the carbohydrate, amino acid and triglycerides composition of the diets administered, and even if they can reverse the inflammatory process.
“Future studies will focus on interventions that can prevent or reverse the damage that develops in the brain with obesity and the possible impact of drugs currently used to treat obesity,” Eroglu said. “Insights gained into dampening this inflammatory process are expected to apply to other tissues such as muscle and bone and hopefully give us insight into how to slow the aging process itself.”
Discoveries at Augusta University are changing and improving the lives of people in Georgia and beyond. Your partnership and support are invaluable as we work to expand our impact.
 Augusta University
Augusta University