Researchers at the Medical College of Georgia at Augusta University are searching for a better way to understand why many men with prostate cancer end up with Alzheimer’s disease, and whether it’s the standard hormone therapy treatment or an overactive immune response that contributes to the problem.
The hormone therapy known as androgen deprivation therapy, or ADT, treats the cancer by reducing testosterone, which the cancer needs to grow. But androgen is a key regulator of amyloid metabolism, and, when it’s removed from the equation, more amyloid is left to form the plaques that are a hallmark of Alzheimer’s.
“We know that prostate cancer itself also largely affects men over age 65, which is a population that’s already at a higher risk of Alzheimer’s, simply due to their age,” said Qin Wang, MD, PhD, Georgia Research Alliance Eminent Scholar in Neurodegeneration and inaugural director of the Program for Alzheimer’s Therapeutic Discovery at MCG. “What is not largely understood is the role ADT may play in the context of cancer and Alzheimer’s disease.”
Wang and her research team suspected that the body’s overactive immune response and subsequent inflammation may be at play.
To better understand, they created an animal model with Alzheimer’s disease and cancer, then delivered the ADT for eight weeks while monitoring androgen levels and tumor size. “We wanted to first validate our model and also check and see if there were cognitive deficits in that group,” Wang said.
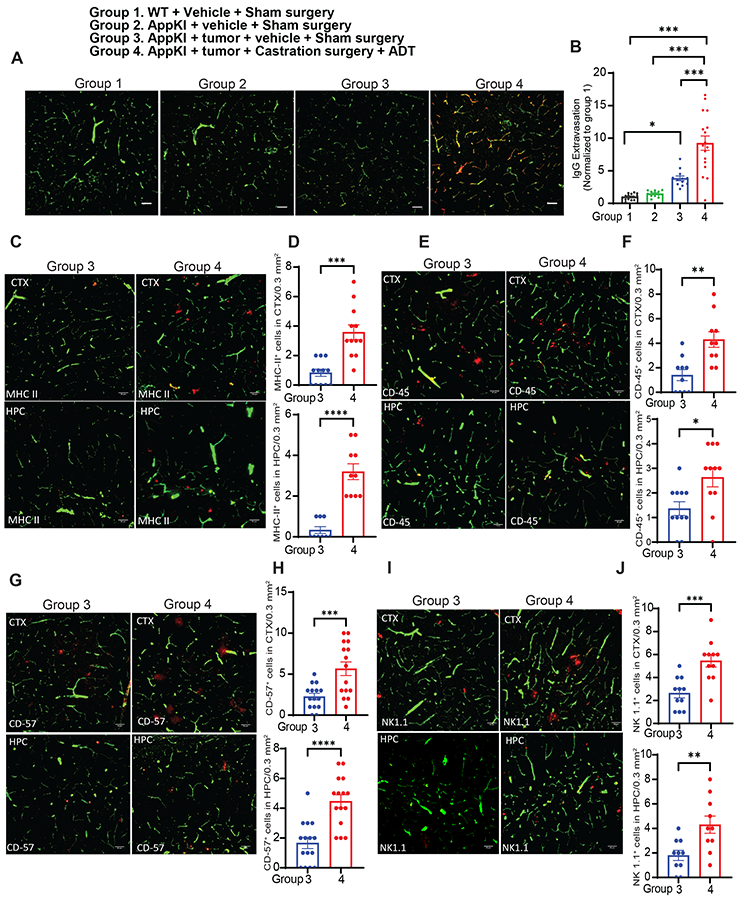
They also developed other animal models. A so-called wild type (without Alzheimer’s or cancer), a group with just Alzheimer’s and a group with just cancer that received ADT therapy helped the team further delineate this complex interplay. The researchers also regularly monitored changes in the blood, looking for immune markers.
At the end of eight weeks, they also looked for increased amyloid in the brain, but “to our surprise we didn’t actually see a significant difference in the plaque load in any of the groups.”
They did, however, note a high amount of reactivity in glial cells of the groups with just cancer and the groups treated with ADT. Glial cells are a part of the central nervous system and typically support nerve cells, helping them function properly. Their hyperactivity is a key indicator of inflammation in the brain, Wang said.
They also noted an increase in pro-inflammatory cytokines, small proteins that trigger an increase in inflammation throughout the body, and a decrease in anti-inflammatory cytokines, particularly in the animals with Alzheimer’s and cancer that received ADT.
The team looked at the animals’ blood-brain barrier and noted that the same group had significant damage. Under normal circumstances, that barrier protects the brain from harmful substances while allowing essential molecules to pass through.
“That would explain why there is so much more inflammation in that group,” Wang and the team reported in the journal Science Advances. “The ADT treatment is actually making the blood-brain barrier more permeable. Then these immune cells, which are circulating in higher amounts because of the cancer and the subsequent treatment, can go into the brain – we call it immune cell infiltration – and cause inflammation, which is associated with cognitive decline.”

To intervene and stop the immune cell infiltration, Wang and her team turned to a drug that is already on the market to treat multiple sclerosis and Crohn’s disease. Natalizumab is a disease-modifying therapy that works by attaching to immune cells and preventing them from moving across the blood-brain barrier and entering the central nervous system.
Treating the mice who had cancer and those who had Alzheimer’s and cancer with a combination of ADT and natalizumab not only reduced the infiltration but subsequently improved the integrity of the blood-brain barrier.
“Then we looked at inflammation markers, and those levels were reduced, as well,” Wang said. “We essentially reduced the pro-inflammatory cycle and improved cognitive function. We now know that it’s not just about the amyloid plaques. The immune system’s response is the contributing factor here.”
Since the drug is already on the market, next steps could include a clinical trial in patients who are undergoing ADT for prostate cancer.
In addition to Wang, the research team included AU graduate student Mae Aida; Shalini Saggu, PhD, an assistant professor in the Department of Neuroscience and Regenerative Medicine; Chao Zhang, MD, PhD, who studies cancer and inflammation at the University of Alabama at Birmingham; and Lizhong Wang, MD/PhD, a professor in the Department of Genetics and the Comprehensive Cancer Center at UAB.
This work was supported with funding from the National Institute on Aging. Read the full study.
Discoveries at Augusta University are changing and improving the lives of people in Georgia and beyond. Your partnership and support are invaluable as we work to expand our impact.
 Augusta University
Augusta University