Scientists from Augusta University’s Medical College of Georgia report that a gene previously implicated in the development of atherosclerotic lesions in coronary arteries could be key to understanding why many people don’t benefit from the most used therapy for neovascular age-related macular degeneration (AMD), a leading cause of blindness.
AMD is a condition characterized by abnormal blood vessel growth in the back of the eye. It is highly prevalent in the elderly and people with diabetes, obesity and many other chronic metabolic diseases. Excessive vascular growth damages the macula, the part of the eye that translates light into image signals.
Anti-VEGF therapy, which blocks vascular endothelial growth factor and keeps excessive blood vessel growth at bay, is usually the first line of defense.
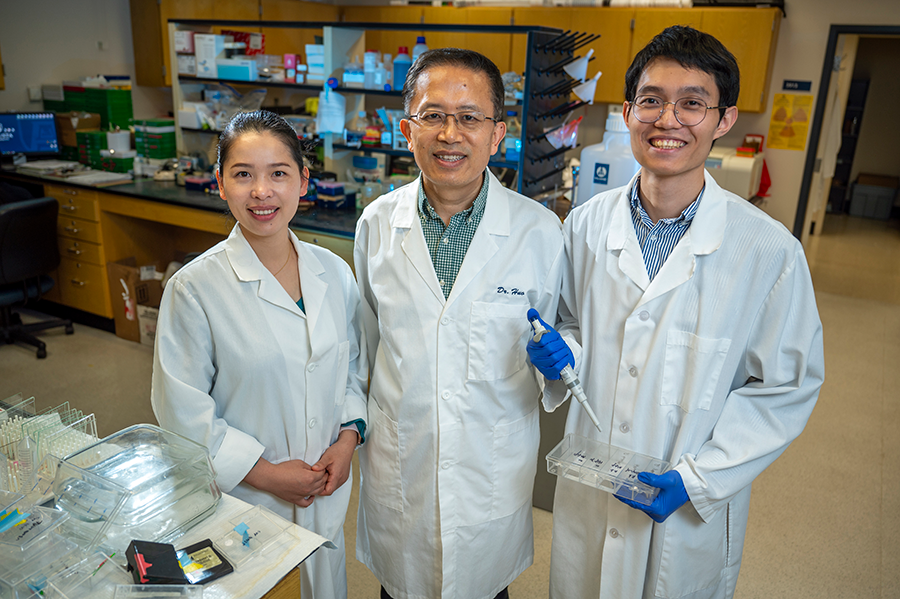
But that treatment only works well for around a third of patients suffering from this form of AMD, said Yuqing Huo, MD, the director of the Vascular Inflammation Program at MCG’s Vascular Biology Center.
“The reason is that the excess vasculature is often accompanied by the growth of fibroblast cells,” he said.
Collagen and many other proteins produced by these fibroblast cells accumulate outside the vascular cells and eventually lead to fibrosis or scarring in the eye. This keeps the excess vasculature from being suppressed by anti-VEGF treatments.
“We show, for the first time in this study, that many fibroblast cells are actually produced by these excessive endothelial cells. We must find a way to prevent this from happening,” Huo said.
He and his team believe the answer lies in targeting the adenosine receptor 2A (Adora2a) — a G-protein-coupled adenosine receptor found in high levels in the brain, immune cells, and blood vessels. Adora2a has been reported to be crucial in modulating inflammation, myocardial oxygen consumption and coronary blood flow. Adenosine, a metabolite produced by cells under conditions of stress, injuries and lack of oxygen, can activate Adora2a to protect our body from injury.
But, in excess, adenosine can lead to excessive blood vessel growth. In their current research, Huo and his colleagues found that a high-level or persistent adenosine-activated Adora2a signal could transform endothelial cells, the luminal cells of the vasculature, into activated fibroblast cells and, eventually, cause fibrosis. Huo and his colleagues hypothesize that blocking this receptor can prevent that from happening.
Using genetically engineered mice that develop fibrosis in the backs of their eyes, researchers delivered an Adora2a agonist (KW6002), which binds to the receptor and blocks its function.
“We also studied mice that had Adora2a removed from only the vascular endothelial cells,” said Qiuhua Yang, PhD, a postdoctoral fellow with Huo and the first author on this study. “All of these mice demonstrated decreased fibrosis in the eye.”
These novel findings were reported and recently selected as the cover image for Science Translational Medicine.
“We have previously demonstrated that blocking Adora2a can reduce excessive blood vessel growth, which happens in the early stages of AMD,” said Yongfeng Cai, PhD, a postdoctoral fellow in Huo’s lab and a member of the research team. They now have an eye toward generating an antibody that could recognize Adora2A.
“The antibody could be delivered via an injection to the back of the eyes, an approach often used in eye clinics, to block the activation of adenosine to Adora2A,” Huo said. “An antibody could really block both excessive blood vessel growth, the early stage of AMD, and fibrosis, the late stage of AMD. Our findings indicate that blocking Adora2a can certainly target multiple stages of this disease, which might be much more efficient than current treatments.”
This research was supported by a National Institutes of Health K99 award to Yang and funds from the National Eye Institute.
 Augusta University
Augusta University




