Magnetic stimulation of a group of nerves that are key to how our gut and brain communicate may help correct the conversation that goes awry in painful, debilitating diabetic gastroparesis, researchers say.
Patients come to Amol Sharma, MD, because their stomachs constantly hurt, they are always nauseous and they can’t or won’t eat or drink. Sometimes they can’t get out of the hospital because of nausea and vomiting.
“Gastroparesis is suspected in about 2% of the population, which is about the population of Missouri, but only confirmed in .2% of the population so it’s a rare disorder,” said Sharma, gastroenterologist at the Medical College of Georgia at Augusta University and AU Health System specializing in neurogastroenterology and gastrointestinal motility.
It’s also not well understood, but physicians like Sharma are beginning to find that it’s a dysfunction in the two-way communication between the gut and the brain. More common problems like irritable bowel syndrome also are thought to be a disorder of this gut/brain interaction, he noted.
Sharma’s lab has developed a painless, noninvasive magnetic stimulation therapy called ThorS-MagNT, which they are using to target and reset the hyperactive firing of a small group of nerves at the midback, a sort of midpoint of communication between the stomach and the brain. He has good evidence from a small pilot study that one-hour sessions targeting this nerve group for five successive days can significantly reduce the disease’s debilitating symptoms.
Sharma recently received a three-year, $958,000 grant (RO1-DK133520) from the National Institute of Diabetes and Digestive and Kidney Diseases to conduct a larger trial.
For the new study, he’s looking at 45 patients and using two different treatment doses, as well as a “sham” control, which looks like magnetic neuromodulation, to more objectively determine how well the treatment works, as well as the optimal dose and placement of the treatment device. That includes looking directly at the impact on nerves both for evidence of change and to better understand how the therapy works.
The MCG researchers are targeting a group of spinal nerves in the midback, which line up with the bottom of the shoulder blades. The nerves make up the celiac ganglia, nerve bundles that are part of the autonomic nervous system, which controls functions we do instinctively like breathing and which get our gastrointestinal tract moving so food moves along as it should.
Sharma describes this region as a sort of midpoint of communication between the stomach and the brain, the pathway that says you are nauseous, full and that you are having pain.
“These are nerves that are easily excited and firing quite a bit and you can change that threshold by repeated magnetic stimulation so that their thresholds are reset so they don’t fire so quickly and so easily,” he says.
He thinks it’s the right target because he thinks dysfunctional nerve function in the stomach is key. The region is also accessible. Interestingly, some of the drugs that have worked best for gastroparesis have been low doses of antidepressants which block some signals from the stomach to the brain, he says. Tests have indicated that some areas that get messages from the gut have extreme responses from essentially no activity to hyperactivity.
The bottom line is that signals from the stomach to the brain are hyperactive which makes signals coming back from the brain say to slow the stomach down. Just why the brain would think that is a helpful response is unclear.
Their pilot study did not include a “sham” control group, or studies of the activity of the nerves directly. Rather they gauged treatment impact from extensive daily diaries patients filled out after dinner about nausea, how many times they vomited in the past 24 hours, how full they felt before even eating and their pain level, all cardinal symptoms of gastroparesis.
Patients consistently told Sharma that their nausea and vomiting were better, and they were ready to enjoy a meal again for the first time in a long time. “Their life is essentially back to normal,” he said.
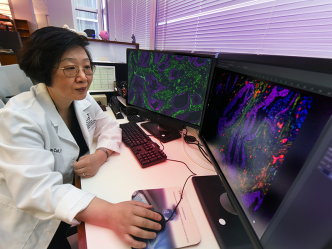
This time they are doing baseline studies of brain activity using sophisticated functional imaging and high-resolution, direct measurement of electrical activity and follow up studies to see if and how it changes.
The focus for these studies is a small area of the brain called the insula, which is increasingly understood as an area which is in touch with all your organs and reaches out to other brain areas as well, which takes Sharma back to the brain likely sending some bad messages to the stomach in gastroparesis.
“The disconnect there is the nerves going from the stomach to the brain for whatever reason are not relaying the right messages. They may be firing too much when maybe they shouldn’t, he said. In an ironic vicious loop, if the gut is sending a signal that you’re nauseous, feeling full real fast and vomiting — classic symptoms of diabetic gastroparesis — then the brain sends a signal back to the stomach to slow down its movement, and the small bowel and gut sometimes get the same message.
“There is a generalized dysmotility of the gut,” Sharma said, that he thinks magnetic stimulation can directly address. If their findings continue to hold, the researchers plan to move forward with a Phase 2 trial with Food and Drug Administration approval ultimately in mind.
There is only one FDA-approved medicine for gastroparesis, called Reglan or metoclopramide, that is said to speed up the stomach and work on nausea centers in the brain. Some patients take antinausea medicines used by patients on chemotherapy for cancer, but the available approaches don’t appear to really address the fundamental communication problem.
Diabetes is a major cause for gastroparesis, but it also can follow surgery, and some medications can trigger the problem. This new treatment strategy should help, regardless of the cause, Sharma said.
“Imagine yourself a patient with diabetes, and you count how many calories you are eating and carbs you are eating, and you give yourself the right amount of insulin to cover these carbs to prevent them from raising your blood sugar. Then the food gets in your stomach, and you end up vomiting up all the food because you are so nauseous and because your stomach doesn’t tolerate it very well,” he said.
Blood sugar levels will go up and down and back, which can make you dizzy, blur your vision, leave you confused, drowsy and make you pass out or worse.
“We have patients arrive in comas because of how high their sugars are, but their low sugars can be just as problematic and serious,” he said.
Blood glucose levels that are too low for too long, starving the brain of glucose, can lead to seizures, coma and very rarely death, according to the American Diabetes Association.
The visceral afferent neuropathy associated with diabetic gastroparesis is when the nerves that sense activity in the abdominal cavity, like the stomach being full from just eating a big meal, are damaged and/or weak. Several studies have shown this occurs in diabetic gastroparesis, along with overstimulation of the sympathetic nervous system with associated nausea.
These nerves communicate fullness, for example, to the spinal cord which takes the information to the brain. As food moves from the esophagus into the stomach, some of the organ’s muscles relax to let it enter, and lower muscles start mixing the food with digestive juices until the particles get small enough to go into the small intestines and we can absorb the nutrients.
Food travels the esophagus likely in less than a minute, and four hours later, about 90% of the meal you consumed should have moved on out of the stomach, Sharma said.
“If it hasn’t, there is a problem,” he said, which could be a blockage or gastroparesis.
For more information about the study, call the research coordinator at 706-721-9875.
Previous work at MCG and the AU Health System led by Satish S.C. Rao, MD, director of neurogastroenterology/motility and the Digestive Health Clinical Research Center, documented nerve dysfunction in a majority of patients with fecal incontinence and found that magnetic stimulation of nerves that regulate muscles in the anus and rectum improve function and dramatically reduce episodes of incontinence.
The prevalence of diabetes in adults worldwide was estimated to be 4% in 1995 and to rise to 5.4% by 2025, taking the number affected from about 135 to 300 million in that 30-year timeframe, according to the ADA.
 Augusta University
Augusta University