AUGUSTA, Ga. – Like that famous bowl of porridge, when leptin levels are “just right” they help protect our cardiovascular health, scientists say.
This satiety hormone, made primarily by fat cells, is best known for telling our brains we are full. In obesity, leptin levels are high but the brain becomes resistant to its message and the cardiovascular system instead comes under attack.
Too little fat and leptin can create a similar cardiovascular risk.
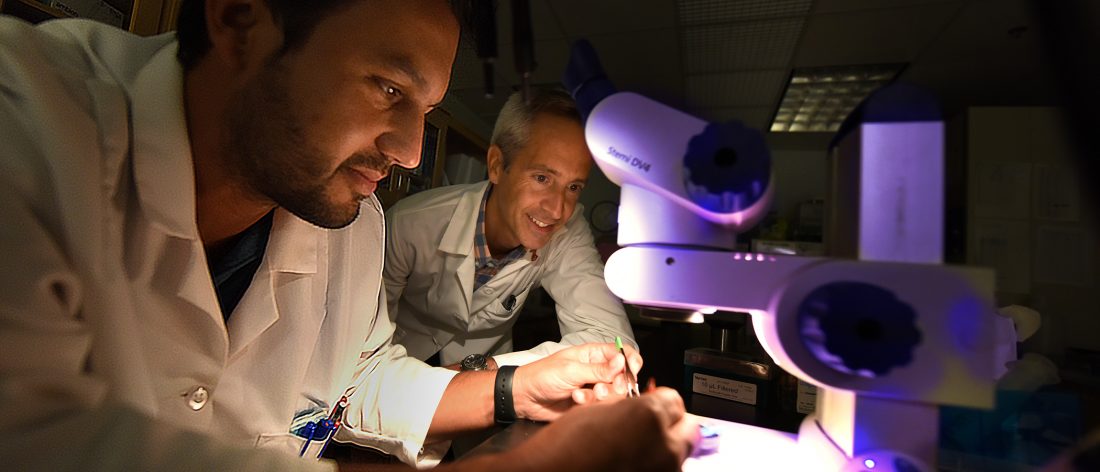
“We need to restore the leptin balance and then we will see its cardiovascular protection,” says Dr. Thiago Bruder do Nascimento, postdoctoral fellow in the Vascular Biology Center at the Medical College of Georgia at Augusta University.
“We think we already have good information that at the right level, leptin protects the cardiovascular system,” says Dr. Eric Belin de Chantemele, MCG physiologist and Bruder do Nascimento’s mentor.
If their studies continue to confirm this, it could point the way toward opening up leptin therapy to a wider range of patients.
Bruder do Nascimento recently received a $965,370 National Institutes of Health K99 grant for postdocs that’s enabling those studies.
They are using a model of extreme leptin deficiency resulting from an extreme fat shortage you can be born with or acquire, called lipodystrophy. While congenital lipodystrophy is rare, infectious conditions like measles or pneumonia, autoimmune diseases, injury, even repeated use of the same injection site for something like daily insulin, can result in acquired lipodystrophy. So can the older but effective antiretroviral therapies for human immunodeficiency virus, or HIV.
Despite the fact that leptin therapy has been prescribed for patients with lipodystrophy since 2014 and the amount given is low, the impact on their cardiovascular system remains unknown, Belin de Chantemele notes.
To create the acquired model, Bruder do Nascimento used a single drug, Ritonavir, long used as an HIV therapy booster, particularly for patients who might not take their medicines as prescribed. He’s finding that after taking Ritonavir for just four weeks, mice develop lipodystrophy and severe vascular dysfunction.
Just one week of leptin therapy reduced the vascular inflammation and significantly improved function, Bruder do Nascimento says. Now they want to know whether it’s a lasting benefit.
They also are learning more about how low leptin hurts the cardiovascular system by looking further at its effect on the single layer of endothelial cells that line our blood vessels.
The cacophony of problems endothelial cells develop just may start with oxidative stress, a byproduct of oxygen use that is damaging at high levels; resulting inflammation; and an impaired ability to help blood vessels relax.
They have evidence that reduced availability of leptin to endothelial cells means the cells help produce less nitric oxide that enables blood vessel relaxation. They’ve shown lipodystrophy also increases oxidative stress, including increased expression of the Nox1 enzyme, which produces the unhealthy byproduct, and reduced PPARy, a receptor involved in good things like reducing bad cholesterol and lipid levels whose loss is associated with higher blood pressure and vascular disease.
The higher oxidative stress produces inflammation, which attracts more immune cells and more inflammation.
Both the endothelial cells and the smooth muscle cells that form the outer wall of blood vessels have chemokine receptors, which are stimulated by the oxidative stress and which help attract those immune cells.
“If you have an inflamed blood vessel, you have activation of this receptor and this receptor sends the message that we have to have more immune cells here,” Bruder do Nascimento says. The immune cells, in turn, secret substances called cytokines, which induce endothelial dysfunction and damage.
They have watched leptin therapy normalize the unhealthy scenario. When they removed what they consider a primary instigator by scavenging for reactive oxygen species with drugs like a Nox1 inhibitor, it also restored endothelial cell function and reduced inflammation.
The MCG scientists have evidence that in blood vessels, leptin somehow decreases chemokine receptors and the ligands that activate them and helps stop the flood of immune cells to the scene. It has the added benefit of decreasing glucose and lipid levels, both of which are cardiovascular risks when high. But in this scenario, decreasing glucose, for example, does not appear to directly result in cardiovascular protection, Bruder do Nascimento notes.
“The effect of leptin directly on the vessel seems to be preventative,” he says.
Now they are learning more about how and really if leptin controls immune cells moving into blood vessels. Interestingly leptin deficient mice are actually more susceptible to infection despite the onslaught of immune cells, Belin de Chantemele says. “It’s turning up inflammation, macrophages and your T cells but in a bad way,” he adds of leptin’s duplicitous role.
A possible problem with leptin therapy could be that the mice, previously unaccustomed to higher leptin levels, actually end up losing weight because of increased signaling to their brain that they are full. Ironically, while obese individuals become insensitive to leptin’s satiety signal those with less fat, and less leptin, are more sensitive to it, Belin de Chantemele notes.
An American Heart Association postdoctoral fellowship awarded to Bruder do Nascimento in 2017 enabled studies in an animal model of lipodystrophy that helped him dissect the reality that while leptin therapy was considered good for other major health problems associated with lipodystrophy, including liver failure, it remained unclear what the therapy did to patients’ increased cardiovascular risk.
The Food and Drug Administration approved a leptin analogue for lipodystrophy in 2014, following evidence that it improved blood sugar levels and lipids and shrank enlarged livers.
The new grant also will help Bruder do Nascimento transition from a postdoc position to a faculty position.
 Augusta University
Augusta University