
Target Market: Who Are They, What Do They Value, and Where Are They?
In last week’s column on Super Bowl ads, I stressed the importance of providing a value proposition when you are advertising or marketing your goods and services. As a reminder, a value proposition is a promise that you make to potential customers that provides them a compelling reason why they should buy your product rather than a product from one of your competitors. Prior to developing a value proposition, you first need to understand who you are trying to sell to and what product characteristics they value. This will ensure that your value proposition will be more likely convince these buyers (your target market) to buy from you. The most effective Super Bowl ads from last week did this important work well. Once the company has a good, valuable proposition, it then needs to communicate that valuable proposition to its target market. Fortunately for companies with Super Bowl ads, just about all target markets are watching the game. However, for pretty much all other advertising and marketing, it must communicate where the target market will see or hear it. In today’s column, I will walk you through how to determine who your target market is, what they value, and finally, where to distribute your marketing messages. You are probably asking yourself, why is a guy who teaches Operations and Supply Chain Management (O&SCM) writing about Marketing? The answer is simple, really. It is the job of the O&SCM function of the company to deliver on the value proposition. So, as marketing develops its value proposition, it must confer with O&SCM to determine if the firm can deliver on that value proposition. If marketing communicates a value proposition it cannot meet, the company will likely be unsuccessful. With that in mind, let us examine the target market/value proposition development process. As a firm begins to identify its target market for a particular product, it must first determine the various potential customers who might buy that product and attempt to partition those customers into groups who value similar things. For instance, looking at the automobile market, there are some customers who value low price most, some who value performance and aesthetics most, and others who value reliability, durability, and consistency. If we are either in the automobile market or thinking about entering the automobile market, we need to find a group that values some characteristics that we think we can provide better than other market entrants. As you can see, the identification of a target market and the development of a value proposition that will appeal to that target market are done concurrently and iteratively. As noted above, the O&SCM function of the company is also brought in during these iterations to determine if the physical good can be manufactured or a service can be delivered in such a way that it can meet the value proposition. One important thing to remember is that in most cases, you are not your target market. What I mean by that is that you are often biased by your own knowledge and taste/preferences, and this may differ significantly from what your target market values. Remember that you are a unique individual whose preferences for a price point and evaluation of other characteristics might differ from your target market. Be sure to develop a value proposition that reflects the buying habits of your target market customers. Once you have developed a strong value proposition that you know your O&SCM can deliver upon, it is time to message that value proposition in places where your target market is present. As noted above, this aspect of our process is like “shooting fish in a barrel” for Super Bowl advertisers because all target markets are typically watching the Super Bowl. It is not so trivial for the rest of us. We need to understand what forms of media our target markets consume (e.g., television, radio, social media), but also, with each of these media, which applications or types of shows do they frequent. While most think social media skews young, and that is true for the most part, Facebook skews older, while Instagram, Snapchat, and TikTok skew much younger. On television, much of network television skew older, but there are shows like “Dancing with the Stars” and The “Bachelor” that do particularly well with younger women. Many mornings when I am getting ready for the day, I listen to “Augusta’s Morning News” on WGAC radio, and it is clear that my fellow listeners are primarily in my age demographic. My advice is to do your homework and find out where your target market is consuming media. All the work above is not very easy, but doing it right will lead to big returns. If you can identify who you want to target, based on what they value, and then be sure they get the marketing message that you have what they value, your business will succeed!
February 24, 2026
4 min

Augusta University public health experts discuss building recovery through economic stability
In this candid conversation, Vahé Heboyan, PhD, and Marlo Vernon, PhD, talk about their work at the intersection of public health, economic stability and substance use disorder recovery. The interviews are centered on Augusta University's public health-driven small business training initiative and explore how recovery is strengthened when communities invest in people and provide practical paths to long-term stability. Heboyan, a professor in AU's School of Public Health and a public health expert with a background as an economist, explains that economic vulnerability often hinders recovery, especially in rural areas with limited resources where risk-taking can be costly. He translates economic research into public health practice, emphasizing that small businesses and microenterprises are about providing a sustainable income for individuals and families, not creating large corporations. This stability, he notes, can have a ripple effect, supporting local economies, job opportunities and community resilience. Vernon, whose research focuses on maternal and infant health, as well as substance use disorder recovery, highlights the human side of recovery and the importance of financial security for families. She notes that economic instability can increase the risk of relapse, especially for mothers in recovery who are supporting children. Her insights show that entrepreneurship can be a public health tool, addressing income, dignity, confidence and long-term wellbeing. Both interviews emphasize the key role of community in recovery. Heboyan points out the power of peer support and shared experience, noting how participants use their past challenges as strengths. Vernon agrees, emphasizing that effective public health work requires building relationships and engaging with communities over time, rather than just conducting short-term research. Together, the interviews show that recovery is part of a larger ecosystem that includes economic opportunity, mentorship and community trust. The video illustrates how combining economics, public health and lived experience can create lasting, meaningful impact for individuals in recovery and their communities. Looking to know more? Click on Dr. Vernon's profile below. To connect with Dr. Heboyan, simply contact AU's Communications team via email (mediarelations@augusta.edu) to arrange an interview today.
February 02, 2026
2 min

A Snapshot of the Local Economy: Simon Medcalfe on Growth, Risk, and What Comes Next
At Augusta University’s annual Economic Forecast Breakfast hosted by the James M. Hull College of Business, Simon Medcalfe, PhD, offered a grounded, data-driven look at how the local economy is performing — and what lies ahead. Speaking to business leaders, students and community stakeholders, Medcalfe emphasized the importance of distinguishing real economic growth from inflation-driven gains, noting that while the Augusta region continues to grow, it does so at a measured pace compared to national averages. His presentation framed the local economy as stable and resilient, but not immune to broader forces shaping the U.S. outlook. A key theme of Medcalfe’s remarks was the role of research, innovation and education in sustaining long-term economic health. He pointed to strong gains in research and development across Georgia and highlighted how university-based research directly contributes to regional economic output. According to Medcalfe, investment in knowledge creation remains one of the most reliable drivers of growth, reinforcing the value of higher education institutions as economic anchors. Simon Medcalfe, PhD, is an economist with an emphasis on sports economics, social determinants of health, and the local economy. View his profile At the same time, Medcalfe cautioned against complacency. While regional fundamentals remain solid, he stressed that uncertainty at the national level continues to pose risks. “However, uncertainty abounds in national macroeconomic policy that could negatively impact growth next year,” Medcalfe said, underscoring how unresolved fiscal decisions and policy shifts can ripple down to local economies. Still, his overall outlook balanced realism with optimism. Medcalfe concluded that the Augusta region — and Georgia more broadly — is positioned to weather uncertainty thanks to diversification, investment in early education, and continued research activity. “Overall, Augusta and Georgia are positioned well for economic growth in 2026 with a strong commitment to early childhood education, a diversified labor market and strong research and development,” he said. View the full article 'Annual Economic Forecast Breakfast offers snapshot of the local economy' here: For journalists covering regional economics, workforce development, higher education, or policy-driven growth trends, Simon Medcalfe, PhD, offers clear-eyed analysis rooted in data — and an ability to translate complex economic signals into insight that matters locally. Simon is available to speak with media - simply click on his icon now to arrange an interview today.
December 31, 2025
2 min

From Libraries to Heart Health: Marlo Vernon Takes Cardiovascular Care Into Rural Georgia
Marlo Vernon, PhD, associate professor in the Department of Health Management, Economics, and Policy at Augusta University’s School of Public Health, is leading a creative public health initiative designed to improve cardiovascular monitoring in rural Georgia. Through the university’s Rural Obese At-Risk initiative, Vernon and her team are placing blood pressure monitors in local libraries, allowing residents to check them out just like books. The effort addresses a critical access gap in rural communities where preventive health tools are often limited or difficult to obtain. Vernon’s work focuses on the realities facing communities in the South’s so-called Stroke Belt, where overlapping health conditions significantly elevate cardiovascular risk. View her profile “There are significant chronic disease risk factors in this so-called Stroke Belt. We’ve got high obesity rates. We have family history. We have high rates of diabetes and kidney disease and they all kind of feed into each other to really create this cardiovascular health need in our communities. And women, in general, are just at a higher risk for this,” said Marlo Vernon, PhD. Beyond equipment access, Vernon’s research also examines how people understand and manage their health when traditional care options are limited. The library-based model helps normalize blood pressure monitoring while reducing barriers such as travel distance, cost, and limited clinic availability. It also creates opportunities to study how community-based solutions can improve awareness, engagement, and long-term cardiovascular outcomes. For journalists covering rural health, women’s health, chronic disease prevention, or innovative public-health strategies, Vernon offers grounded, real-world insight into how trusted community spaces can play a vital role in addressing persistent health disparities. A full article on this topic is available below. To arrange an interview with Dr. Vernon simply click on her iconnow to set up a time to talk today.
December 28, 2025
2 min

Why Insomnia May Hold the Key to Treating Depression, According to MCG Research
William Vaughn McCall, MD, professor emeritus in the Department of Psychiatry and Health Behavior at the Medical College of Georgia at Augusta University, is leading a new multi-year clinical trial aimed at addressing insomnia and depression together — two conditions that frequently occur side by side. The Assessing Improvements in Mood and Sleep (AIMS) Trial, funded by the National Institutes of Health, is exploring whether treating sleep problems through psychotherapy can also reduce lingering symptoms of depression, particularly in older adults. McCall has served as professor and Case Distinguished Chairman of the Department of Psychiatry and Health Behavior at Augusta University since 2012. His research interests include depression, electroconvulsive therapy, quality of life, insomnia, and suicide. His research has been continuously funded by the National Institute of Mental Health since 1995, and he is the author of more than 400 publications, including more than 180 peer-reviewed journal articles. View his profile McCall’s work builds on decades of research examining how disrupted sleep contributes to mood disorders. While previous studies often focused on medication-based approaches, this trial takes a different direction by testing non-pharmacological therapies that target insomnia itself. The research team, which includes collaborators from multiple universities, is evaluating whether improving sleep quality can meaningfully lower depression symptoms for patients who remain symptomatic despite antidepressant treatment. “Ultimately, the hope is to find other avenues to reduce the risk for depression and depression symptoms,” McCall says. The trial is currently recruiting adults aged 55 and older who are experiencing both insomnia and depression, with options for both in-person and remote participation. For journalists covering mental health, aging, sleep science, or emerging clinical research, McCall is a key expert offering informed perspective on how sleep-focused interventions could reshape the future of depression treatment. The full article 'New MCG trial targets insomnia and depression symptoms' is available below: And if you're interested in talking with William Vaughn McCall, MD, simply click on his icon now to arrange a time for an interview today.
December 24, 2025
2 min

AU scientists advance understanding of Nobel-winning immunology research
The 2025 Nobel Prize in Physiology or Medicine recognized the discovery of regulatory T cells, which are immune cells that maintain tolerance and prevent autoimmunity. At Augusta University, scientists have built upon that foundational work, uncovering how these cells function, fail and evolve across diseases like cancer and atherosclerosis. Regulatory T cells, or Tregs, are essential for controlling immune responses and preventing the body from attacking its own tissues. Early discoveries by Shimon Sakaguchi, MD, PhD, who identified the CD25 marker and later the transcription factor FoxP3, revealed how Tregs suppress immune activation. Sakaguchi, a distinguished professor at Osaka University in Japan, shared the Nobel Prize with Mary E. Brunkow, PhD, Princeton University, and Fred Ramsdell, PhD, University of California, Los Angeles. Sakaguchi once shared lab space with Nicholas Gascoigne, PhD, now a professor at AU’s Immunology Center of Georgia, where he studies T-cell signaling and differentiation — a connection that ties the global history of Treg research to the university’s ongoing expertise. Gascoigne’s research continues to illuminate how Tregs differentiate and signal, critical steps in ensuring immune tolerance to self. “Drs. Sakaguchi, Brunkow and Ramsdell have made enormous contributions to our understanding of how immunological tolerance works, so this prize is very well deserved,” Gascoigne said. “I was happy I could help Drs. Shimon and Noriko Sakaguchi when they needed lab space back in the early ‘90s. They were wonderful to work with.” At Augusta University, David Munn, MD, co-director of the Pediatric Immunotherapy Program of the Medical College of Georgia at Augusta University, made seminal discoveries showing that Tregs are not always stable. Munn’s team demonstrated that these cells could lose their suppressive identity and become “exTregs,” adopting pro-inflammatory characteristics under certain conditions. Munn also uncovered an entirely distinct tolerance mechanism through indoleamine 2,3-dioxygenase, a pathway independent of FoxP3 that regulates immune balance through tryptophan metabolism. “In particular, the work of Shimon Sakaguchi and Fred Ramsdell was profoundly influential on our early work, as we were just starting out to explore how the immune system is regulated in pediatric cancers,” Munn said. “The work of these Nobel laureates helped transform the scientific understanding of how the immune system responds — or fails to respond — in the setting of tumors.” Catherine “Lynn” Hedrick, PhD, co-director of the Immunology Center of Georgia, further expanded this understanding by showing that Tregs can convert into follicular helper T cells, offering new insight into how immune regulation can shift toward antibody production in chronic inflammatory diseases such as atherosclerosis. “Understanding how regulatory T cells can shift identities helps explain why the immune system sometimes loses balance in chronic disease,” Hedrick said. “By tracing how Tregs convert into other helper cells, we’re uncovering new therapeutic targets to restore immune harmony in conditions like atherosclerosis.” Building on these advances, Klaus Ley, MD, co-director of IMMCG, and his team have investigated how exTregs contribute to cardiovascular inflammation, identifying them in human tissues and clarifying their role in atherosclerosis. His lab also recently discovered human exTregs, providing the first direct evidence of these cells in people. Two postdoctoral fellows in Ley’s lab, Qingkang Lyu, PhD, and Smriti Parashar, PhD, continue this work, exploring how regulatory and ex-regulatory T cells influence chronic disease progression. Additionally, Dimitrios Moskofidis, MD, PhD, a professor based in the Georgia Cancer Center, contributed key early insights into immune tolerance and memory, defining how effector T cells persist or are deleted following infection. “Together, these discoveries place Augusta University and the Immunology Center of Georgia at the forefront of modern immunology, connecting molecular mechanisms of tolerance to real-world diseases and therapies,” Ley said. To connect with any of the experts or researchers in this article - simply contact AU's External Communications Team mediarelations@augusta.edu to arrange an interview today.
December 22, 2025
3 min
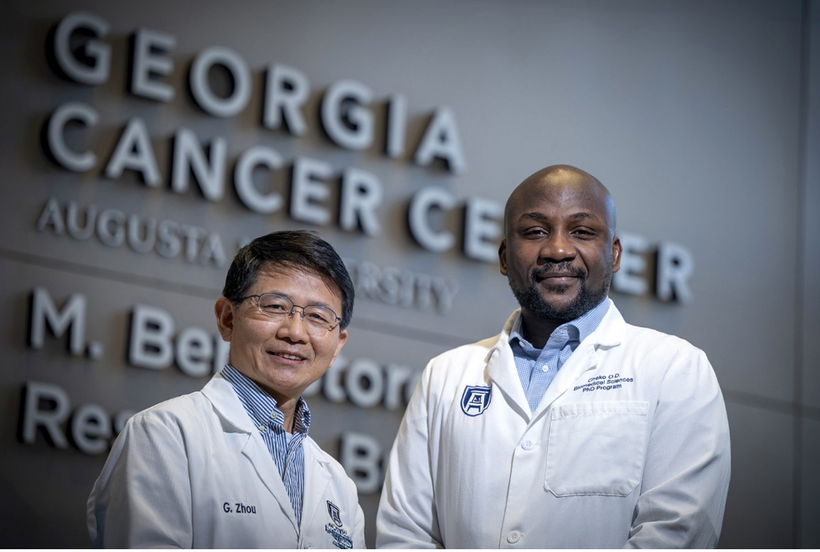
Fueling the Future of Cancer Immunotherapy: Gang Zhou’s Research Takes a Major Step Forward
Cancer immunotherapy has transformed how clinicians approach the treatment of certain blood cancers, but major limitations remain — especially when it comes to sustaining strong, long-lasting immune responses. Gang Zhou, PhD, a leading cancer immunologist at Augusta University’s Georgia Cancer Center and the Immunology Center of Georgia, is tackling these challenges head-on. Zhou’s work focuses on how T cells behave inside the body and how their performance can be enhanced to improve patient outcomes. His lab studies the forces that strengthen or weaken T cell responses, including their functional status, their ability to self-renew and the environmental pressures they face inside tumors. This deep understanding positions him as a key figure in the effort to advance next-generation immunotherapies. Recently, Zhou and his research team were awarded the first Ignite Grant from the Immunology Center of Georgia — a seed program designed to support bold, high-impact translational ideas. Their funded project aims to make CAR-T therapy more effective. CAR-T is a type of immunotherapy in which a patient’s own T cells are genetically modified to recognize and attack cancer cells. While this approach has revolutionized the treatment of certain blood cancers, it still faces obstacles such as limited cell persistence and reduced strength over time. “Our ultimate goal is to engineer T cells that not only survive longer but also remain highly functional, giving patients more durable protection against their disease.” Zhou’s team is addressing this issue by studying how a modified form of STAT5, a transcription factor that plays a key role in T cell survival and function, may help engineered T cells last longer and perform better. The ultimate goal is to create CAR-T therapies that maintain potency, withstand the harsh tumor microenvironment, and offer durable results for patients. The Ignite Grant recognizes not only the promise of this specific project, but also Zhou’s broader expertise in understanding how T cells can be guided, supported, and strengthened to fight cancer more effectively. His research contributes to a growing wave of scientific innovation aimed at improving immunotherapy outcomes for patients with both blood cancers and, potentially, solid tumors — an area where current treatments face significant barriers. As immunotherapy continues to evolve, the work led by Gang Zhou stands as a compelling example of how foundational science, translational research, and clinical ambition can work together to push the field forward. To connect with Dr. Gang Zhou - simply contact AU's External Communications Team mediarelations@augusta.edu to arrange an interview today.
December 16, 2025
2 min
MCG scientists investigate arthritis drug’s impact on Alzheimer’s disease
According to the Alzheimer’s Association, more than 7 million Americans are living with Alzheimer’s disease, and one in nine of those people is 65 or older. Although that number is expected to grow, researchers at the Medical College of Georgia at Augusta University are making progress on studies that could turn into life-saving treatments. Qin Wang, MD, PhD, professor in the Department of Neuroscience and Regenerative Medicine at MCG and Georgia Research Alliance Eminent Scholar in neuropharmacology, recently published a study titled “The PKCι‑β‑arrestin2 axis disrupts SORLA retrograde trafficking, driving its degradation and amyloid pathology in Alzheimer’s disease,” in Molecular Degeneration, a leading journal in neurodegeneration. In the study, Wang and her team explored how certain proteins and enzymes interact in the brains of Alzheimer’s patients. Key players include the SORL1 gene, the PKCι enzyme and proteins SORLA, β‑arrestin2 and amyloid. SORL1 encodes SORLA, which helps regulate amyloid. Amyloid can form plaque in the brain, contributing to Alzheimer’s. People with the disease often have lower SORLA levels, which amplifies plaque production. “The goal is to increase SORLA levels in patients with AD. If we can boost it up, that would be great,” Wang said. “But if you want to know how to boost it up, you have to know how it is degraded, so that’s what our work is about – we’re trying to understand how its stability is regulated.” Wang’s research team found that PKCι can add a phosphate group to SORLA, which helps SORLA interact with β‑arrestin2. The PKCι‑β‑arrestin2 axis leads to SORLA degradation, reducing its levels and allowing amyloid plaques to grow unchecked, thereby worsening the disease condition. They discovered this by using biochemical methods and a mass spectrometer managed by Wenbo Zhi, PhD, at the Proteomics and Mass Spectrometry core lab at AU. “We conducted biochemical studies and found that SORLA can be phosphorylated. We identified the phosphorylation site and the interacting enzymes,” Wang explained. “Using the mass spectrometer with PKCι, we saw increased phosphorylation of SORLA at certain sites. Preventing that could stop SORLA degradation.” That’s where a rheumatoid arthritis drug called auranofin comes into play. “While it is an arthritis drug, it can also inhibit the PKCι enzyme,” Wang explained. The team conducted tests using Alzheimer’s mouse models and human iPS cells developed into neurons. For the mouse models, they treated the mice with auranofin for eight weeks, resulting in decreased amyloid levels, reduced neuroinflammation and improved cognitive function. Similar results were seen in human cells with increased SORLA levels and decreased amyloid levels. “A good thing about this is, because this is an FDA-approved drug, it’s ready to be tested in Alzheimer’s patients,” Wang said. “People often worry about drug safety because of long-term use in chronic diseases like Alzheimer’s, but, in this case, existing safety data for chronic use gives a good starting point for testing in Alzheimer’s patients. “I hope a drug company can pick that up for a trial with Alzheimer’s patients because we are trying to translate our bench work all the way to the bedside for treatment,” she continued. The study wraps up a five-year National Institute on Aging grant, a collaborative effort between Wang’s lab and the Kai Jiao, MD, PhD, lab in AU’s Center of Biotechnology and Genomic Medicine. Wang’s team is also working on other grant-funded Alzheimer’s-related projects and hopes to continue making advancements toward finding a cure for this debilitating disease. “All of our projects share the goal of finding a better treatment,” Wang said. “Related to this project in particular, we want to know how the SORLA protein works in different types of brain cells, given the brain’s complexity. Then we can determine how to specifically target that protein to develop more effective therapies.” Qin Wang, MD, PhD, researches the neuropharmacology and signaling mechanisms underlying neurological and psychiatric disorders. If you're interested in learning more about her work or booking an interview, simply click on her icon now to arrange a time to talk.
November 04, 2025
3 min

Experts in the Media: CBD may help treat and reduce inflammation in Alzheimer's disease
In a recent Medical News Today article, Corrie Pelc reported on a study led by Babak Baban, PhD, in which inhaled CBD (cannabidiol) was tested in a mouse model of Alzheimer’s disease to examine its effects on neuroinflammation. Baban, associate dean for Research with AU's Dental College of Georgia and a professor with appointments in neurology and surgery in the Medical College of Georgia at Augusta University, explained that previous work from his group showed inhaled CBD to be more effective than oral or injected forms for certain neurological conditions, motivating them to explore its potential in Alzheimer’s research. He emphasized that Alzheimer’s is driven by multiple interacting biological processes – not just amyloid plaques – and sees inflammation as a promising new therapeutic target. In the study, inhaled CBD lowered activity in two major immune “alarm” pathways – IDO (indoleamine 2,3-dioxygenase) and cGAS-STING – both implicated in chronic inflammation. By dampening these pathways, CBD reduced levels of inflammatory cytokines and helped restore a more balanced immune environment in the brain. Baban framed this as a shift from symptom treatment to addressing underlying immune dysfunction, and noted that the findings could reorient how Alzheimer’s is approached. At the same time, he stressed that human trials are still needed: his team is preparing translational studies and holds an active Investigational New Drug (IND) application with the FDA for inhaled CBD in neuroinflammatory conditions, with Alzheimer’s disease as a natural next step. Read the full article here: Babak Baban, PhD, is a professor, immunologist and associate dean for research at the Dental College of Georgia at Augusta University where he has served for 13 of his 20 years as a translational and clinical immunologist. View his profile here Looking to know more about this important research or to connect with Babak Baban, PhD? He's available to speak with media – simply click on his icon to arrange an interview today.
October 29, 2025
2 min
 Augusta University
Augusta University