We’ve all been there: sitting in the waiting room for a long time, hoping to hear your name called.
One graduate student in the College of Allied Health Sciences took notice of this and decided to dig deeper.
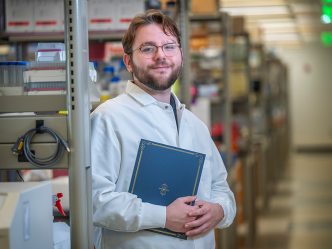
“For some patients, long wait times required sitters, it was taking them out of their job, and the patients weren’t getting the treatment they needed,” said Scott Stevens, who earned a Masters of Public Health from Augusta University in 2017. “I was starting to notice that was a big issue.”
After delving into this further, he and his mentor Assistant Professor Dr. Vahé Heboyan hypothesized that there might be an increase in patient visits due in part to changes in mental health at different times of the year.
He decided to take a look at the data on patient visits to emergency rooms due to mental and behavioral issues through the seasons, from 2013 to 2015, as part of his Capstone Project.
Dr. Vaughn McCall, department chair for Psychiatry and Health Behavior at the Medical College of Georgia at Augusta University, brought in his expertise after hearing about it.
They wanted to see if there was a correlation between depression and the various seasons, or if there was a correlation with the change of time that comes with daylight saving time.
“I read that mental illness can be aggravated by changes of the season,” said McCall, on what interested him in the project. “Some folks believe that you’re more likely to have mania in the summer and depression in the winter. There’s plenty of evidence that abrupt changes in the way people sleep during daylight savings time can cause insomnia and car accidents, among other things.”
The trio looked at the two weeks before and the two weeks following a time change.
“We found things that weren’t what we expected,” said McCall.
For example, despite there being a variation in mental health-related visits to the emergency room, there was no real correlation between winter and depression (or warm weather and mania) in the results.
And as for daylight saving time, “It did increase the number of visits right after DST starts,” Heboyan said. “The change of the clock starts to affect your health.”
However, the patterns were inconsistent, perhaps due to the limited nature of the study with visits only to Augusta University Health. Though the findings were ultimately inconclusive, they saw this as just the beginning and believe there is reason for further study. They believe the data may also suggest that socioeconomic factors could play a larger part in mental health visits to emergency rooms.
The research, which started as a Capstone Project, was published in the American Journal of Emergency Medicine.
“Publication was never in the forefront of my mind,” said Stevens, who now works in radiology at University Health Care System. “It was great to watch the project evolve into what it became. It was great that you can get that kind of investment from the faculty.”
Heboyan said that the inclusion of McCall was crucial to the project.
“When you bring someone like Dr. McCall, whose career is in behavioral health, who can advise you — that creates a much more rigorous article in research outcomes,” he said. “He helped us make interpretations that you might not have thought about because you are not subject experts in the field.”
All three of them hope that this is just the beginning for this area of study.
“I believe we have something there, but we were limited to a single site,” said Stevens. “My hope is someone will take the research and apply it to other regions of our country and other countries.”
 Augusta University
Augusta University