About 17% of women with unexplained infertility also have gene variants known to cause disease, from common conditions like heart disease to rare problems like ALS, Medical College of Georgia at Augusta University researchers report.
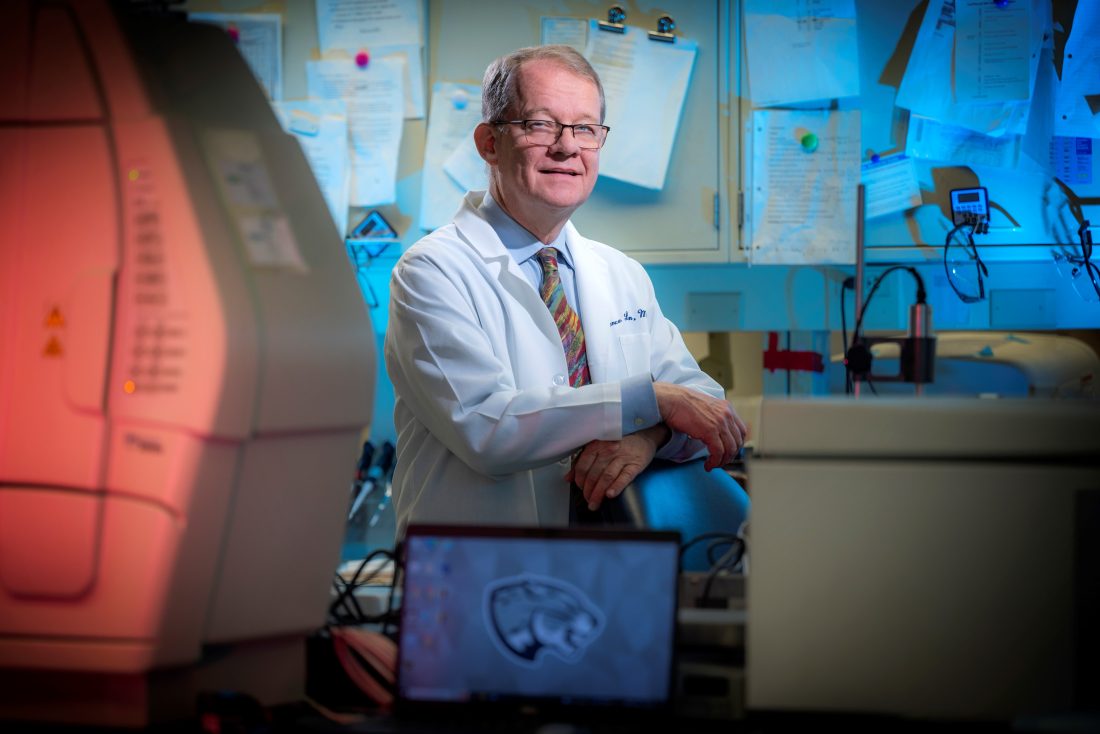
Theirs appears to be the first study to identify an increased prevalence of disease-causing genetic variants in females with unexplained infertility, the team, led by Lawrence C. Layman, MD, reports in the New England Journal of Medicine.
They hypothesized that genetic disease creates a predisposition to infertility and subsequent medical illness and their findings support that link, they write. Females with infertility, for example, have been noted to have an increased risk of cardiovascular disease.
“The connection to diseases has been known, but what has not been known was if there was a genetic connection. That was the purpose of this study,” says Layman, a reproductive endocrinologist and geneticist who is chief of the MCG Section of Reproductive Endocrinology, Infertility and Genetics.
The investigators note that while clear, common pathways between infertility and conditions like heart disease, still have not been established, “a strong association between infertility and future disease can still assist in early detection, genetic counseling and intervention.” Fertility could be in effect a “biomarker” for future medical illness, they write.
They sequenced the exomes, which contain the protein-coding regions of genes, of 197 females ages 18 to 40 with unexplained infertility, a percentage that comprises about 30% of infertile females, to look for variants in genes that were known or suspected to cause disease.
Information on the women was pulled from the AMIGOS Trial of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Cooperative Reproductive Medicine Network, a group of some 900 couples from multiple institutions with no obvious cause for infertility, like problems with ovulation or unhealthy sperm.
They found 6.6% of the females they studied had variants in 59 genes termed “medically actionable,” which means they are likely to cause conditions like heart disease and breast cancer but there are interventions, lifestyle and/or medical, that might remove or at least reduce their risk. By comparison about 2.5% of the general population have been found to have variants in these genes.
An additional 10% of the females had gene variants known to cause disease for which little to no action could be taken to ameliorate the problem, like Parkinson’s disease, Layman says.
They found 14 variants of the medically actionable genes in 13 of the females; one woman had two variants. The most common were those that contribute to cardiovascular disease and cancer, the nation’s top two killers.
Those included relatively well-known variants, like four women with variants of BRCA1 and BRCA2, which are associated with a high risk of breast or ovarian cancer. Six females had variants in five genes associated with the increased risk of cardiovascular disease, things like having a genetic predisposition to high cholesterol levels and irregular heart rhythms, some of which can be lethal.
One female had a variant in the gene MYH11, which is associated with increased risk of a rupture of the aorta, the largest blood vessel in the body. Numerous rare variants of uncertain significance also were found in the medically actionable genes.
Comparatively large datasets that better represent the entire population, like 50,000 people in the United Kingdom Biobank and nearly 22,000 in the National Human Genome Research Institute-funded eMERGE network, yielded percentages of 2 and 2.5% respectively.
That translates to about a threefold increase in variants in medically actionable genes among the females who were infertile compared with the general population, Layman says.
Additionally, they found 20 variants in 21 other females in genes associated with conditions that likely could not be mitigated, like a dramatically increased risk of developing muscle wasting ALS, or Lou Gehrig’s disease, and kidney-destroying polycystic kidney disease, which will ultimately require dialysis and/or a kidney transplant, a finding that requires more study, Layman and his colleagues write.
All told about 17% of the females with unexplained infertility had variants that are known to cause or suspected to cause a future medical illness. They note that their findings are likely relevant only to this group of women.
While more study is needed before moves are made like recommending genetic testing for all females or males with unexplained infertility, the investigators say their findings support the notion that the higher incidence of future medical problems in these women may have a genetic component.
At the moment, genetic testing in infertility is done selectively, such as if the suspected problem points to a genetic cause, like a male having no sperm, which may indicate Klinefelter syndrome, where males are born with an extra copy of the X chromosome that results from a random genetic error.
“We don’t do genetic testing right now because there hasn’t been good evidence for it and it’s not going to be covered by insurance,” Layman says. Their new study provides more evidence that genetic testing might need to be considered a handful of years down the road if findings continue to hold.
“We need to study a lot more people and other people need to do that too,” Layman says.
Another area that needs further exploration is whether some of the gene variants may be causative of both infertility and disease, Layman says. Right now, the only variants familiar to him that appear to have a role in both are cancer-causing BRCA 1 and 2, because they also are involved in meiosis, which is important to sperm and egg formation and function. They also are both involved in repairing double-strand breaks in the DNA, which has been associated with ovarian aging and cancer risk, Layman says.
Another is a variant that causes early menopause, which is known to increase the risk of heart disease, because estrogen is considered protective of the female cardiovascular system.
He hopes the new findings will inspire others to further explore whether the disease-causing variants they found present in these females also are factors in their infertility.
Layman also notes that the database they studied happened to be largely white females, but that infertility is a problem common to both Blacks and whites as well as other races, and needs to be studied in these populations.
Infertility also affects men and women equally, according to the American Society for Reproductive Medicine.
One of Layman’s many pursuits include a larger study that also includes males. He wants to do genetic studies on couples then continue to follow them past the point of their seeking reproductive help to specifically assess when and if diseases associated with the genetic variants they found start to surface.
While Layman has some patients that he follows long term, most of his patients come to him during the years they are working toward having a child while some of the conditions, like breast cancer, that can result from the gene variants they found, tend to occur a decade or more later. He has wondered about what happened in his patients’ lives long term because of associations that have been made between infertility and a handful of diseases.
When the National Institutes of Health issued a funding opportunity in 2020 for research exploring infertility as a marker for overall health in light of increasing evidence that “fertility status can be a window into overall health,” he decided to further explore the associations.
Dr. Michael Diamond, a reproductive endocrinologist who is senior vice president for research at AU, is a longtime principal investigator on the National Institute of Child Health and Human Development Cooperative Reproductive Medicine Network. Diamond enabled the university to join the cooperative, designed to enable large clinical trials that improve the diagnosis and treatment of reproductive health issues, a decade ago when he came to MCG and AU from Wayne State University in Detroit. Diamond is a coauthor on the new study in the NEJM.
Michael P. Dougherty, MD, who completed his reproductive endocrinology fellowship with Layman and is now in practice in New Jersey, is first author.
Today 72 genes are considered medically actionable by the American College of Medical Genetics and Genomics.
Read the full study.
 Augusta University
Augusta University