Peripheral artery disease, or PAD, in which impaired blood flow to the legs can make walking painful and even lead to amputation, and negative social determinants of health, like poverty and racism, both disproportionately affect older Black adults.
Now physicians want to further explore the relationship between the two conditions to identify social determinants of health that may be a factor in nearly doubling the rates of PAD in Blacks compared with other racial or ethnic groups, especially in the Southeast.
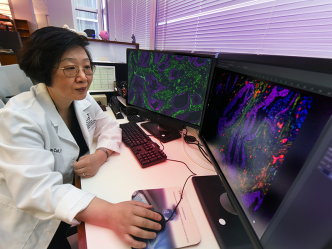
“African Americans are more likely to have the disease, they are less likely to have it diagnosed and, if diagnosed, they are less likely to receive appropriate therapy, which can result in irreversible, lifechanging events like leg amputation,” says Monique Bethel, MD, cardiologist at the Medical College of Georgia and AU Health.
Poor social determinants of health, things like food and housing insecurity and low educational attainment, have been found to directly increase the burden of other blood vessel diseases like heart disease and stroke and their risk factors, according to the Centers for Disease Control and Prevention. And PAD shares risk factors, like high cholesterol and high blood pressure, with both those conditions.
Still, while a blood pressure measure on the arm is standard at most doctor visits to see if hypertension, for example, is present, a measure of pressure at the ankle to look for insufficient blood flow to the legs is not, Bethel says.
And there are mixed recommendations regarding screening for PAD by national panels, with the U.S. Preventive Services Task Force, for example, saying there is no direct and limited indirect evidence that screening of unselected or asymptomatic individuals is of benefit, Bethel says. Meanwhile, the American College of Cardiology and the American Heart Association have joint practice guidelines recommending screening with the ABI, or ankle brachial index, which looks at blood pressure in the ankle as an indicator of blood flow, in patients at increased risk, including adults 65 years or older, adults 50 years or older with risk factors for atherosclerosis or a family history of PAD, and adults younger than 50 years with diabetes and one other risk factor for atherosclerosis.
There also are calls for more studies to better determine when and whether screening can improve outcomes. And, the U.S. Preventive Services Task Force also says that screening might benefit some groups.
Bethel wondered if Blacks might be one of those groups.
“We know there are clear risk factors for this condition,” she says. Being Black is already on that list and she suspects that social determinants of health should be as well. “If we know they have the disease, we can attack their risk factors more aggressively,” she says.
Bethel and her colleague Vishal Arora, MD, director of the Peripheral Vascular Intervention Program and Interventional Cardiology at MCG and AU Health, are screening patients who come to the general cardiology clinic or peripheral vascular disease clinic, as well as inpatients admitted to the cardiology service at AU Medical Center.
They are looking for individuals that meet similar criteria to the American College of Cardiology guidelines, which includes those 65 and older, those 50-64 who are smokers or have diabetes, and those under age 50 who are smokers and have diabetes.
The new study will not include those who already have been diagnosed with PAD or who have clear indications of the disease like gangrene or nerve damage in their legs as well as indicators of blood vessel disease elsewhere like the heart and brain.
The methods they are using to look for PAD are painless and will be completed in just one visit. They are checking blood pressure in the arm and comparing it to the pressure at the ankle with the ankle-brachial index test to make the diagnosis. The top number should be about the same in both locations and if it’s lower at the ankle it means something is obstructing blood flow. “Literally the blockages are stopping the blood flow from getting there,” says the study’s principal investigator Bethel.
While the ankle-brachial index is considered diagnostic for PAD, it doesn’t indicate exactly where the plaque is found. A Doppler ultrasound can help determine location.
They also are using a brief Centers for Medicare and Medicaid survey designed to assess social determinants of health, which are defined as conditions in which people are born, grow, live, work and age, which impact socioeconomic status, education, employment, your neighborhood, social support and access to health care.
“One of the questions is: Do you worry about a place to stay? Another: Do you worry about getting food?” Bethel says. The survey also assesses mood symptoms and Bethel is adding a question about educational attainment level.
She wants to see if certain determinants of health are regularly present in Blacks who screen positive for PAD, versus those who do not, as way to begin to collect objective evidence about whether together they paint a picture of a clearly at-risk population that could benefit from screening. It may also help fine-tune Black individuals most at risk and help narrow proposed screening, she notes.
“We already know it’s more prevalent among African Americans, but could we do better, could we catch it earlier?” she says.
Improving outcomes, is clearly a bottom line. Those, for example, who are at risk may be able to make lifestyle changes that will at least slow or halt disease progression like getting regular physical activity, stopping smoking, striving to improve emotional health and controlling and/or preventing diabetes.
She notes, for example, that when you don’t feel your neighborhood is safe, you may not feel comfortable walking or running in it. Physical activity has provided some of the best benefit to people with PAD says, so the investigators’ many goals also include development of a home-based exercise program.
“We don’t know exactly why exercise works like it does, but we do know it improves overall vascular health, it improves the way the blood vessels work, it raises good growth factor and good cholesterol. It works,” Bethel says.
PAD is more common in Blacks than any other racial or ethnic group, according to the National Institutes of Health, potentially because related conditions like high blood pressure and diabetes, also are more common. Other known risk factors include smoking, high cholesterol and having blood vessel disease elsewhere in the body, like the heart. Smoking and diabetes appear particularly problematic in PAD. Blacks also are more likely to experience negative social determinants of health like polluted water, racism and violence.
Although many of us think of blood vessel disease in the heart and brain, PAD can happen throughout the thousands of miles of blood vessels in the body, but tends to be most common in the legs, where fat and cholesterol deposits narrow the passageway for blood.
PAD can make limbs cool to the touch, muscles atrophy and slow hair growth on the legs, as well as cause pain and cramping in the legs and buttocks that typically subsides with rest, poor wound healing and gangrene. But it also can be asymptomatic, at least in the earlier stages, and any pain experienced in the legs and buttocks, may get attributed to other issues, including age.
“People develop chronic wounds, they can’t walk far. A lot of these patients end up with amputations, or even dying,” Bethel says. “It’s a disease that is really underrecognized, understudied and undertreated, but it has a profound effect on patients.”
About one in every 20 Americans over the age of 50 has PAD, according to the National Institutes of Health. Up to about 40% of patients have both PAD and heart disease, Bethel says. “Different people get different ones first and some may never get both.” The heart, or coronary artery disease, is typically discovered first, primarily because patients are more aware of this top killer in the United States and caregivers regularly look for it, she says.
Brian Annex, MD, cardiologist and chair of the MCG Department of Medicine, whose research focus has long focused on PAD, encouraged Bethel to do this first study to develop sufficient pilot data to do a much larger study to better understand and treat this common condition, whose risks are shared with some of the nation’s biggest killers.
If you would like to participate in the study, please call the MCG Division of Cardiology at 706-721-4997.
 Augusta University
Augusta University