AUGUSTA, Ga. – More typically, these immature immune cells might help us fight cancer, but scientists have now shown cancer can commandeer the cells to help it spread.
Cancer uses myeloid-derived suppressive cells, or MDSCs, that come from the bone marrow, like a support system to successfully metastasize, report scientists at the Georgia Cancer Center at Augusta University.
While cancer early and often sends out cells from its primary site – like the lungs or breast – to other organs, most cells don’t survive immune system surveillance. Still, 90 percent of cancer deaths are related to metastasis.
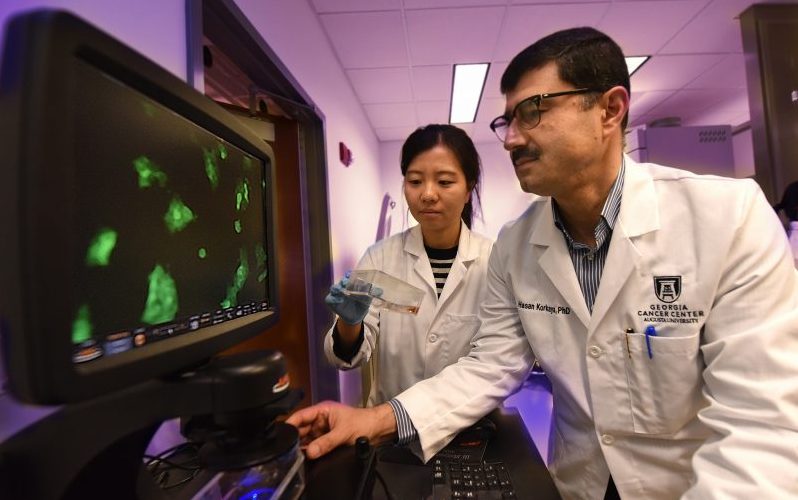
“These cells are essential to successful cancer metastasis,” said Dr. Hasan Korkaya, molecular and cancer biologist at the Georgia Cancer Center and Medical College of Georgia at Augusta University.
While it’s known MDSCs, found in high levels in mouse models and patients with cancer, are good at suppressing the immune response, their role in enabling tumors to spread and succeed is emerging, said Korkaya, corresponding author of the study in the journal Nature Communications. Dr. Maria Ouzouonova, who just completed her postdoctoral fellowship in Augusta, and fourth-year graduate student Eunmi Lee are co-first authors on the study.
It’s thought that the tumors cells about to leave the primary site become stem-cell like so they can free themselves from the primary tumor, and more easily migrate to and populate a new area. Once there, they revert to a state that enables them to take up residence.
The new study shows commandeered MDSCs aid both: One type – monocytic MDSCs – help tumor cells make the stem-cell like transformation while another– granulocytic MDSCs – helps them essentially revert, settle in and grow.
MDSCs appear to get their wayward direction from cytokines, in this case, secreted by the tumor. Cytokines are small signaling proteins normally secreted by the immune system to influence other cell types. But a tumor also can secrete these chemical messengers, and the message it sends to these immature myeloid cells is to support it.
“They are being schooled toward facilitating tumor cell growth and metastasis,” Korkaya said. Like bad parents, tumors also use cytokines to keep the MDSCs from maturing so they can keep telling them what to do.
“There is a very intricate balance in the immune system that is usually anti-tumorigenic, meaning it eliminates tumors, but in some cases, if this balance is altered, these cells may actually help tumors grow and develop into full-blown metastatic disease,” Korkaya said.
Even prior to the newly published study, Korkaya strongly suspected that a cocktail of certain cytokines would enable tumors to turn the suppressive power of MDSCs to their advantage. In his earlier mouse work at the University of Michigan, for example, Korkaya was among the first to show that when he used an antibody to eliminate cytokine IL-6, it significantly reduced metastasis of breast cancer in mice. Anti-IL-6 therapies are now in clinical trials.
He’s not yet certain whether MDSCs travel with migrating tumor cells or if they are an advance team that readies their future remote location. But when he looks at tumor cells in his current mouse model of breast cancer, the ones that have taken hold in a new organ are surrounded by MDSCs.
Rather than eliminating the large volume of wayward cells, Korkaya and his research team are already exploring ways to re-school them to fight rather than support tumors. That includes finding ways to target cytokines found in high levels in metastatic disease.
Most of us without cancer have low levels of MDSCs and very few circulating in the blood, rather they tend to be undifferentiated cells waiting, mostly still in the bone marrow, for a call to action, like a bacterial infection or tumor.
MDSCs also are known to be a major impediment to successful immunotherapy, in which agents are used to strengthen the ability of the patient’s immune system to battle cancer. In fact, recent studies have suggested that MDSCs may have to be eliminated for immunotherapy to be optimally successful, Korkaya said. The cells also appear to have a role in angiogenesis, or helping tumors form blood vessels they need to survive once they reach a certain size.
Some types of cytokines are actually used to treat cancer and/or to offset other negative effects of chemotherapy, like helping make more healthy red blood cells in response to the loss of these cells that occurs with treatment.
 Augusta University
Augusta University