Syed Adeel H. Zaidi, PhD, an assistant research scientist who studies retinal neurovascular biology in the Vascular Biology Center of the Medical College of Georgia at Augusta University, has received a prestigious grant from the Knights Templar Eye Foundation for his research on blindness in premature infants.

“This grant is a great honor and step in my career as a researcher since it is my first grant,” Zaidi said. “I am very appreciative of my mentor, Ruth Caldwell, PhD. She’s well established in studying the retinopathy of prematurity, and I appreciate her guidance and insight as I launch my own research projects. Having been able to work with her and the rest of our team has been very beneficial.”
According to the Knights Templar Eye Foundation Inc., somewhere in the world, a person goes blind every five seconds, with over 7 million people going blind every year.
The Knights Templar Eye Foundation supports research that can help launch the careers of clinical and basic researchers focused on the prevention and cure of potentially blinding diseases in infants and children. They support clinical or basic research on conditions that can be treated and may eventually be prevented. Examples include but are not limited to amblyopia, congenital cataract, congenital glaucoma, retinopathy of prematurity, ocular malformations, congenital nystagmus and other hereditary eye diseases such as retinal dystrophies or retinoblastoma.
Retinopathy of prematurity (ROP) is among the most common illnesses that affect premature or low birth-weight infants and is a major cause of long-term vision impairment and blindness. ROP is a disease that damages the vascular and neuronal parts of the retina, causing infants to go blind.
Zaidi notes that the current clinical standard of care provides some relief; however, many children have a loss of vision even after completing those therapies. Zaidi’s research is aimed at developing a novel therapy to limit neuronal and vascular damage in ROP patients.
“When a baby is born prematurely, there are many organs which are not fully developed, including their lungs and retinas, and for their survival, neonatologists put them in oxygen chambers in order to support their lung development,” Zaidi said. “This oxygen-rich environment inhibits the development of their retinal vessels. Once their lungs are more developed and the infants are taken out of those chambers into a less-oxygen-rich environment, their retinas suffer from hypoxia due to the lack of retinal vessels, and this causes their vessels to develop abnormally and also damages the developing retinal neurons.”
Zaidi noted that during pathologies, the human body starts making specific metabolites in excess that cause more harm than benefit.
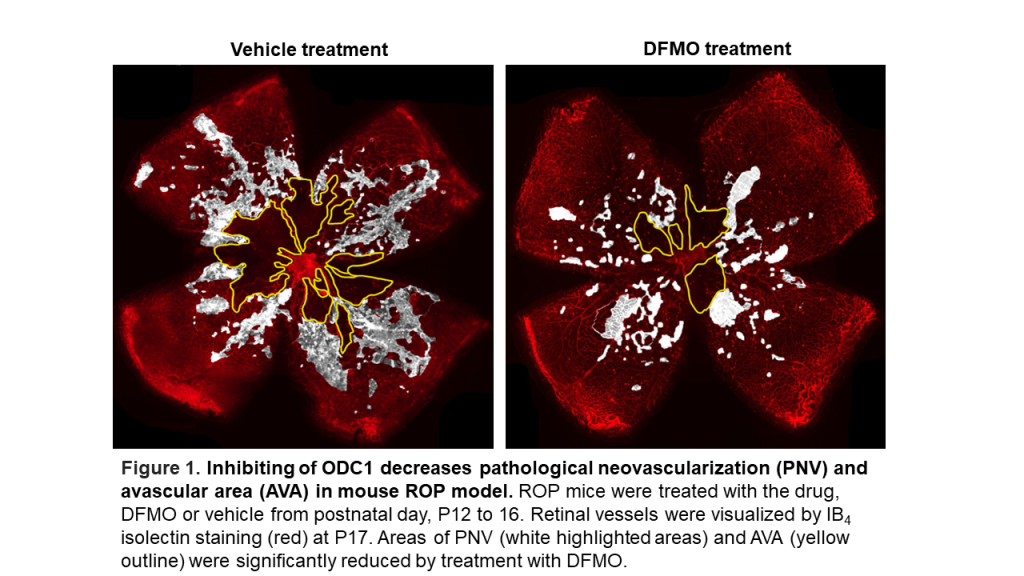
“We have discovered a previously unrecognized enzyme, ornithine decarboxylase 1 (ODC1), that is overactivated in ROP and causes toxic levels of polyamines in the retina.” Zaidi said that he believes using an ODC1 inhibitor called difluoromethylornithine (DFMO, commercially known as Eflornithine), which is an FDA-approved drug used in the treatment of Alzheimer’s and other diseases that they can rescue the neurovascular injury.
The new grant will aid Zaidi in testing his treatment in a pre-clinical mouse model before seeking approval and funding to move on to clinical testing.
“We will use this drug in a mouse model of ROP and test whether it helps to promote normal vascular development and preserve their visual function. Based on this study, we can repurpose this approved medicine for a clinical trial in ROP infants. We hope this medicine will help the infants recover from such a blinding disease and preserve their vision,” Zaidi said of his study, titled “Targeting the ornithine decarboxylase 1/polyamine pathway to limit pathological neovascularization in retinopathy of prematurity (ROP).”
Zaidi is also first author on a similar study, which is aimed at stopping vision loss in premature newborns.
READ MORE: Medical College of Georgia scientists work to protect the vision of premature babies
Zaidi joined the Ruth Caldwell Lab as a postdoctoral fellow in December 2020. Caldwell is a renowned leader in the retinopathy field with an outstanding record for training postdocs to become independent investigators. She is a part of the Vascular Biology Center and the James and Jean Culver Vision Discovery Institute at Augusta University.
Caldwell’s research has focused on the role of arginase in ischemic retinopathy and traumatic optic neuropathy. Her work showed that targeting the arginase pathway offers a novel strategy for limiting retinal neurovascular injury and promoting repair during these conditions.
 Augusta University
Augusta University




