Sometimes a “no” can lead someone to look in a different direction for a “yes.”
That is the case for Ali Arbab, MD, a professor in the Department of Biochemistry and Molecular Biology at Augusta University’s Medical College of Georgia who has spent most of his career studying breast cancer.
When one of his proposed methods for treating breast cancer didn’t result in a grant, Arbab shifted the focus to other diseases and found he could tailor his methods to help stroke victims. This resulted in Arbab receiving a $423,500 grant from the National Institute of Neurological Disorders and Stroke (NINDS), part of the National Institutes of Health (NIH).
“I have spent much of my career focusing on studying breast cancer, but when I developed this new technology for treating cancer, I knew it could be used for treating other diseases. With that knowledge, I did exactly what the technology can do and re-focused my attention to how it can be used to treat stroke patients, and I was able to secure this grant,” Arbab said.
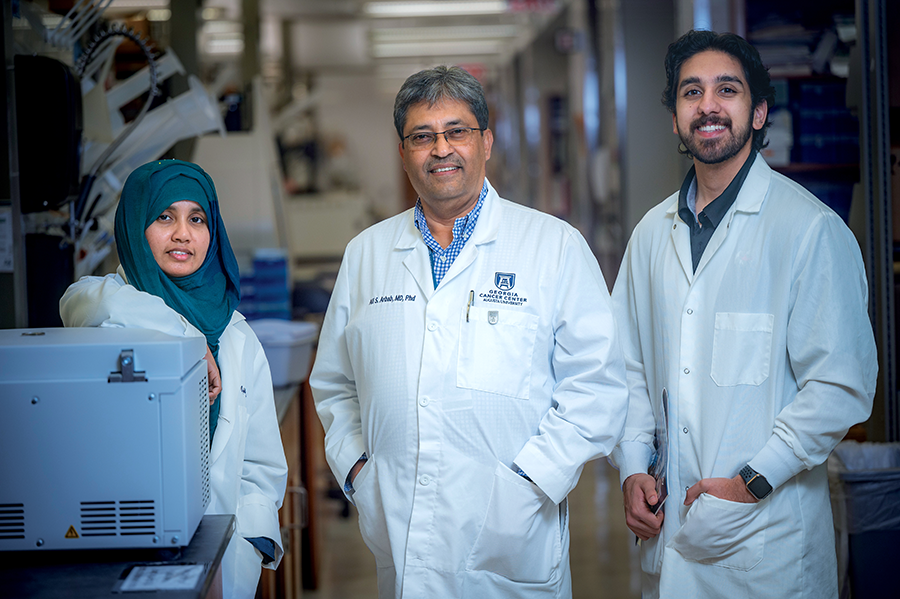
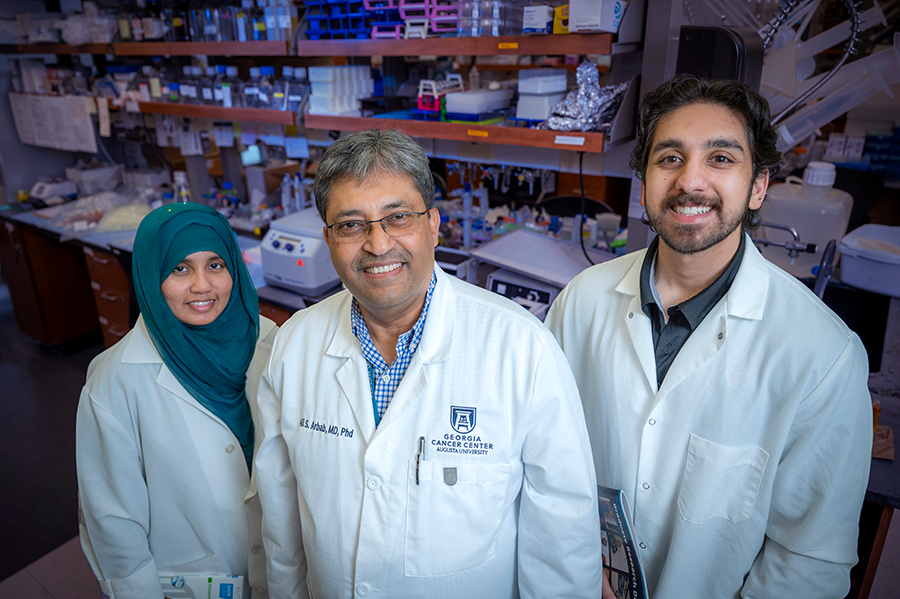
Arbab and his team, which includes researcher Sawaiz Kashif and graduate research assistant Mahrima Parvin, have developed a DNA technology platform to make engineered exosomes using non-tumorous HEK293 cells that can accept targeting, as well as therapeutic payloads for targeting specific cells in the body. Arbab has utilized specific cell-targeting peptides derived from the rabies virus, specifically neuron-specific rabies virus glycoprotein (RVG), as well as neuroglobin (Ngb), a therapeutic probe/payload to protect neurons from hypoxic/ischemic and oxidative stress-related insults following ischemic stroke.
But there are more barriers to overcome, and that’s time. The minutes and hours following a stroke are some of the most critical in treatment, and Arbab found that the best window for the treatment to be administered is within the first six hours after the onset of a stroke, resulting in the search for a way to deliver the treatment more efficiently.
The team tried administering the treatment via injection through the bloodstream initially, but it still wasn’t making it in sufficient numbers to the brain due to the blood-brain barrier.
To that end, Arbab and his team have shown enhanced delivery of the exosomes to the sites of stroke using pulsed-focused ultrasound (pFUS) without causing damage to the surrounding brain tissues. While the IV injection is being administered, the team uses ultrasound in the area to help enhance the delivery of the exosomes. It does risk damaging more brain tissue, but ultrasound has the ability to be fine-tuned to minimize the side effects.
“The great thing about ultrasound is it can be tuned to a frequency that does not damage any part of the brain but rather increases permeability through the blood-brain barrier to allow admission of the treatment,” Arbab said. The pFUS is administered through an intact skull over the stroke site of the brain.
Preliminary results from another of Arbab’s studies also showed that enhanced delivery of EPC exosomes by pFUS caused significantly decreased stroke volume and improved cerebral blood flow over 28 days compared to that of EPC exosomes only.
 Augusta University
Augusta University