We know that too much body fat is generally bad for our cardiovascular system, and now scientists are learning more about how too little fat yields some of the same damage.
Their goals include determining whether leptin replacement therapy for people born with a rare condition, where they have little body fat, helps protect their cardiovascular system. They also want to learn if it might do the same for those with conditions like HIV infection and autoimmune disease, who lose healthy fat stores later in life.
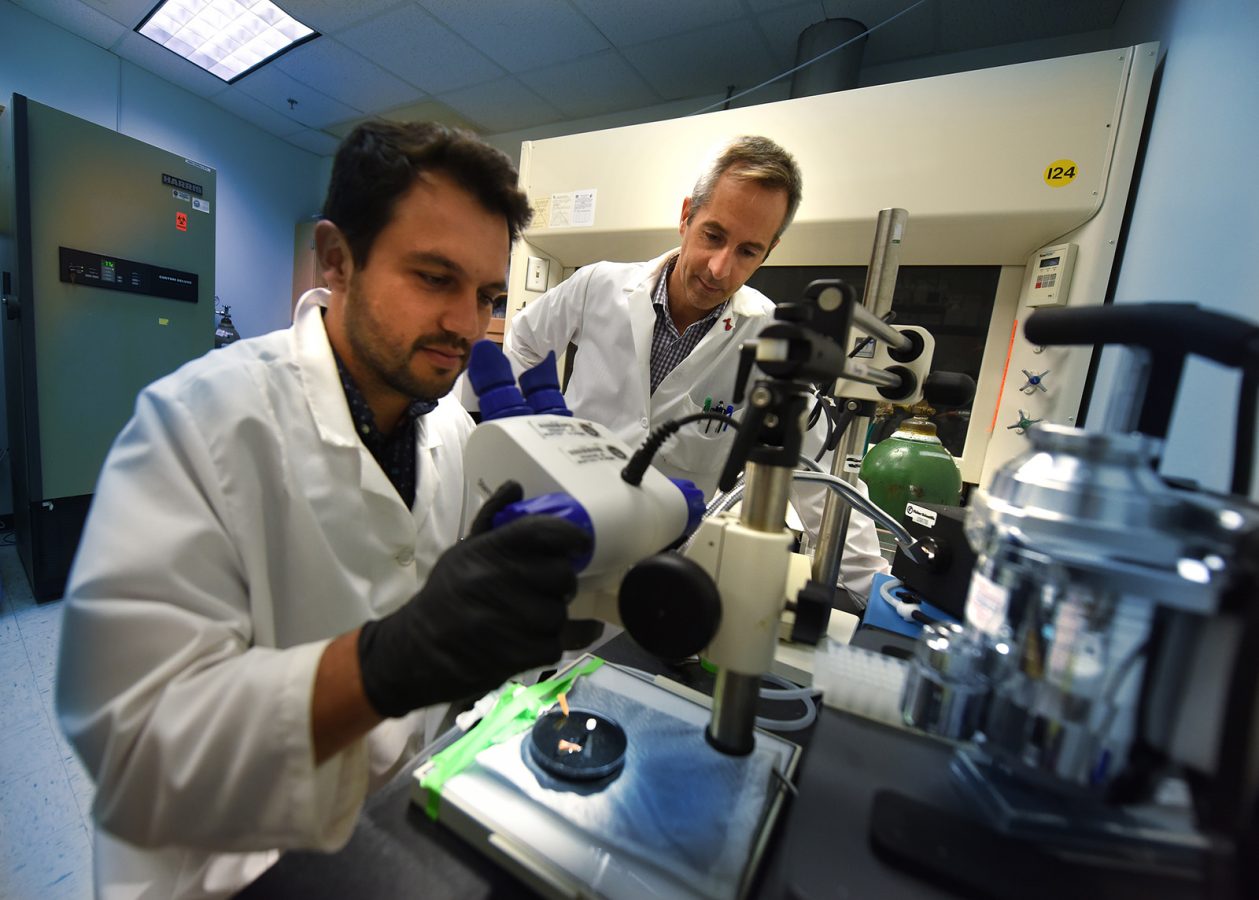
Congenital lipodystrophy is the polar opposite of obesity but has similar damaging consequences for the cardiovascular system, said Dr. Thiago Bruder do Nascimento, postdoctoral fellow in the Vascular Biology Center at the Medical College of Georgia at Augusta University.
A key factor appears to be the extreme levels of the satiety hormone leptin – high in obesity, low in lipodystrophy – found in each, says Bruder do Nascimento, who recently received a $102,550 postdoctoral fellowship award from the American Heart Association to explore the impact of leptin therapy on cardiovascular health in lipodystrophy.
Fat is the major producer of leptin, which helps regulate fat storage and use, and is increasingly considered a key factor in cardiovascular health.
In the case of congenital lipodystrophy, patients have little fat and leptin, Since the lipids, or fats, they consume have no logical place to go, they pile up in places like the liver, heart and muscle. The unnatural accumulation is bad for the individual organs and – like obesity – increases the risk of diabetes and cardiovascular disease, Bruder do Nascimento says.
“These patients would develop atherosclerosis and heart disease, and liver failure is one their major causes of death,” says his mentor, Dr. Eric Belin de Chantemele, physiologist in the Vascular Biology Center and associate professor in the Department of Medicine at MCG.
A leptin analogue, approved by the Food and Drug Administration in 2014 for congenital and generalized lipodystrophy, reduces high levels of blood sugar and lipids as well as dangerous liver size in these patients. It also seems to stabilize their appetite, which, despite their lack of fat, is tremendous.
“We improved their metabolic function, we reduced their appetite, we reduced their glycemia, but what is the effect of this treatment on their cardiovascular system since high leptin levels are bad for the cardiovascular system,” Belin de Chantemele says.
Numerous studies, including those by Belin de Chantemele’s team, have detailed the ill effects of high leptin on the cardiovascular system. For example, his team reported in 2015 in the AHA journal Circulation that high leptin levels directly activate high levels of the steroid hormone aldosterone, which is known to contribute to widespread inflammation, blood-vessel stiffness and scarring, enlargement and stiffness of the heart and impaired insulin sensitivity.
While the amount of leptin given to lipodystrophy patients is relatively low, the therapy’s impact on the cardiovascular system is largely unknown. But the MCG scientists have early evidence that it is good.
In a mouse model of lipodystrophy, they find similar pathology to that found in humans: less fat and leptin, increased tendency of blood vessels to contract and impaired function of endothelial cells that line the vessels and enable relaxation. They’ve found leptin replacement therapy restores healthy glucose levels and endothelial function and reduces excess contractility. Now they are learning more about how.
One of the many jobs of endothelial cells is to produce eNOS, the precursor for nitric oxide, a powerful dilator that enables blood vessels to relax. Bruder do Nascimento is finding that in lipodystrophy, there is increased expression of the NOX1 enzyme, which produces high, damaging levels of reactive oxygen species. They are learning more about the effect of high reactive oxygen species levels on endothelial cells, like whether they directly reduce nitric oxide levels or interfere elsewhere.
Early lab evidence suggests leptin replacement therapy brings levels of both NOX1 and reactive oxygen species down so they also want to know how leptin reduces NOX1.
The studies also are enabling them to learn more about the usual relationship between leptin and endothelial cells. Eventually the scientists want to explore what happens to these interactions when they give too much leptin, which they suspect will turn the early positive results they are seeing very negative.
If their findings continue to hold, long-term goals of their AHA-supported work include paving the way for leptin replacement therapy to be available to more patients.
The FDA’s 2014 ruling specifically notes that the injectable drug metreleptin is not indicated for patients with HIV-related lipodystrophy or for those with partial lipodystrophy, like patients with autoimmune disease or infected with HIV might have.
In the case of partial lipodystrophy that may occur later in life, patients lose much of healthy fat normally found on our arms and legs, for example, and instead start packing fat in the belly region and around major organs in the abdominal area, again jeopardizing both individual organ health and significantly increasing cardiovascular risk with this co-called visceral adiposity.
Other recommended treatments for lipodystrophy include regular exercise and a healthy diet. Liposuction may help selectively remove some unhealthy fat pockets.
 Augusta University
Augusta University