It’s something most of us likely take for granted — until we can’t do it.
Swallowing refers to the seemingly simple process that gets food and drink from our mouths to our bellies.
But the process is anything but simple, and for some, with a condition known as dysphagia or difficulty swallowing, it can seem downright impossible.
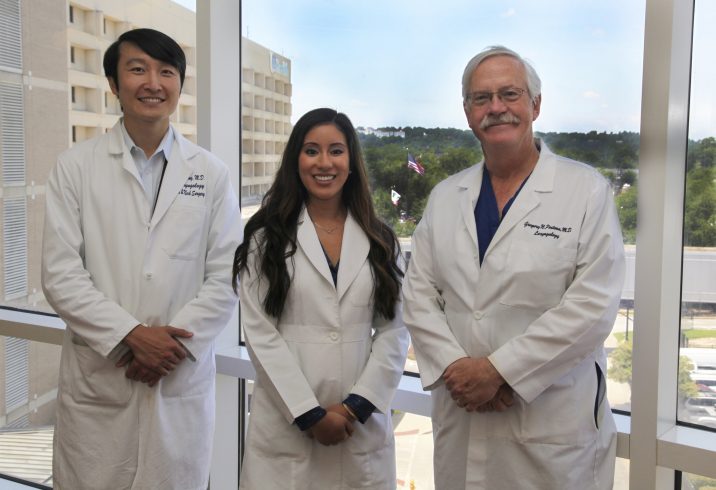
“Swallowing happens in three main phases,” explains Stephanie Reyes, a speech language pathologist in the Center for Voice, Airway and Swallowing Disorders at the Medical College of Georgia at Augusta University and AU Health.
The first phase is the oral phase, when the brain sends messages to the mouth to chew the food, and the muscles there mix it with saliva to form a bolus and move it toward the back of the mouth. During the second, known as the pharyngeal phase, the vocal folds close to keep food and liquids from entering the airway and the tongue and throat muscles push the bolus into the esophagus. In the third and final phase, the esophageal phase, food and liquids move further into the esophagus, which contracts and moves the food into the stomach.
“It’s almost like a relay race from the mouth to the throat to the stomach,” Reyes says. “The baton has to be passed on to the next runner at every step and in a smooth way.”
Dysphagia occurs when that baton is dropped.
“Dysphagia is a symptom though,” says Dr. Mike Yang, a laryngology fellow in the MCG Department of Otolaryngology. “It describes the general issue of difficulty swallowing, but it can have many different causes and can vary in severity, from a mild nuisance to potentially life-threatening problems like aspiration (of food into the windpipe), which can lead to aspiration pneumonia and can cause death.”
People with dysphagia often end up seeking professional help when they experience things like the sensation of something being stuck in their throats, trouble swallowing liquids or solids, coughing when swallowing or recurrent pneumonia, says Dr. Greg Postma, vice chair of the Department of Otolaryngology and director of the Center for Voice, Airway and Swallowing Disorders. “It’s up to us to figure out the cause,” he says. “It’s not uncommon for someone to have multiple causes.”
Some root causes of dysphagia are things like GERD, when stomach acid damages the esophagus; radiation therapy for head and neck cancers, which can cause the muscles and mucosal lining of the mouth, throat and esophagus to become stiff and deformed; Parkinson’s disease, when progressive muscle loss can cause patients to lose control of their mouth and throat muscles; and stroke, when damage to the brain can interfere with getting messages to the mouth, throat and tongue.
The disorder affects an estimated 590 million people worldwide and costs the US health care system over $500 million annually, Yang says. That is a number that is only growing. “The population is aging and the incidence of disorders that result in dysphagia, like strokes, increase as people age. I think it’s becoming a more and more important problem that needs to be addressed.”
Soon it may grow even more.
“I think I think we’ll eventually see an influx from COVID-19 patients,” Reyes says. “You’ve got to take into account that a lot of these patients are getting tracheotomies and being placed on ventilators and (their swallowing muscles) may atrophy.”
Postma says he also has concerns about how the current pandemic could affect future dysphagia patients.
“I’m more worried about people’s fear of COVID keeping them from coming to the hospital,” he says. “My biggest fear is that we’re going to get patients not being properly evaluated. For something like reflux, that may be ok, but we see a lot of cancer at our center. I don’t want someone with swallowing problems that are related to cancer to delay two to four months and end up having a more advanced cancer.”
As with so many other maladies, early detection can help prevent symptoms from worsening and is key to successful treatment.
“I think a lot of times people with mild to moderate symptoms tend to just blow it off. I wish people knew that frequently we can find a cause and we can treat it,” Yang says. “There are things we can do to help even when the symptoms aren’t that severe.”
“Studies have shown that in different cultures, trouble with swallowing or eating has a higher effect on quality of life than loss of voice,” Postma adds. “In people who have lost their larynx to cancer for instance, research has demonstrated, for those patients, their ability to swallow supersedes their ability to talk.”
June is Dysphagia Awareness Month. To reach the MCG Center for Voice, Airway and Swallowing Disorders, call 706-721-4400.
Follow MCG’s Department of Otolaryngology on Instagram and Facebook.
 Augusta University
Augusta University