Two faculty members at Augusta University’s Dental College of Georgia are giving the term “power couple” a whole new meaning.
Ana Carolina Morandini, DDS, PhD, and Erivan Ramos Jr., DDS, PhD, were recently awarded a nearly $2 million grant from the National Institutes of Dental and Craniofacial Research to study the causal relationship between periodontitis, or gum disease, and metabolic dysfunction. The two have collaborated for almost 20 years, having met while pursuing their master’s degrees, falling in love, getting married and starting a family.
Morandini, an associate professor in the Department of Oral Biology and Diagnostic Sciences and the Department of Periodontics, specializes in inflammation and immunobiology of periodontal tissues, whereas Ramos, an assistant professor in Oral Biology and Diagnostic Sciences, focuses on bone biology and osteoimmunology. Their concentrations on oral soft and hard tissues complement each other, especially in this study, for which they are both principal investigators.
“We are approaching the disease both from the inflammatory standpoint and from the metabolic standpoint,” Morandini said. “We’re trying to understand this axis between metabolism and inflammation.”
Morandini’s role is to look at how nucleotide molecules in gum tissue cells can make the environment more pro- or anti-inflammatory and influence disease progression, while Ramos will be looking at how metabolic dysfunction affects bone cell behavior.
“Because the body can form an axis between the gingival cells and the bone cells, that communication between the cells can actually have an impact on how the disease progresses and how it affects the systemic health of the individual. So it can help us better understand how gum disease connects with obesity and metabolic disorders,” Morandini explained.
While it’s known in the dental field that many systemic diseases start in the mouth, the concept has evolved over the years and has become more complex than early research believed. Initially, it was hypothesized that pathogenic bacteria were traveling from the mouth through the bloodstream to other tissues, which Morandini said is true to a certain extent. But some people who don’t even carry certain pathogenic types of bacteria still have gum disease and metabolic disorders.
In fact, some people who have fairly good oral hygiene are still developing gum disease as they age, and, since it is a chronic condition, they will permanently be periodontal disease patients.
“Maintaining a healthy state goes beyond effective control of dental biofilm, which we know has a crucial role in disease, but the response is sometimes disproportionate because of how each individual’s metabolism shapes their overall health,” Morandini said. “So we have the two sides of the coin there.”
To put it in perspective, she claims almost half of the adult population in the United States has some form of periodontal disease, and that percentage rises to 70% when someone is over the age of 65.
“When people start aging, they are more susceptible to bone resorption and chronic diseases, and we don’t believe this is physiological. We don’t believe this is normal, that just because someone is aging, they should get fragile bones, lose bone and have retraction of the gums,” she said. “We believe there are some processes or mechanisms within the cells that we could identify early to make sure these people can have a longer health span of their oral tissues and, therefore, enjoy healthier lives.”

A big focus of the study will be on a little-known enzyme found in the gum tissue called CD73 and how it affects both bone loss and metabolic function. Morandini said the mitochondria, the parts of the cell responsible for generating most of its energy, are the main players when it comes to providing the cell with resilience to delay metabolic disorders. They plan on investigating CD73’s impact on the mitochondria and their ability to protect the cell from aging and stress.
“As much as we can understand the mechanism of how the mitochondria dynamics influence the host response, it’s going to pave the way for us to identify biomarkers to early diagnose gum disease,” she said.
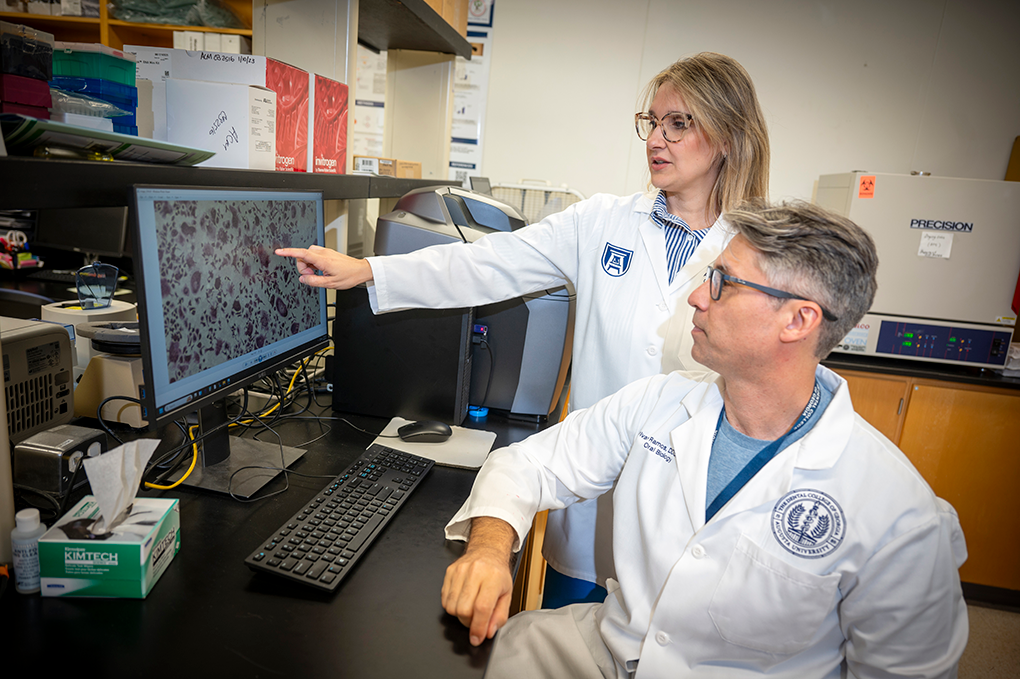
To test their hypothesis, the pair has used an in vitro model to study the impact of inflammatory processes on the cells and an in vivo mouse model to study how metabolic dysfunction can affect the mice’s ability to recover from disease.
To do that, researchers feed the mice high-fat, high-calorie diets to gain weight. They also tie a suture to their back molars so they accumulate plaque and have a high chance of developing gum disease. Lean and obese mice with or without sutures are used as the control variables.
As part of the experiment, the scientists then treat the mice with medicinal interventions in hopes of preventing them from developing the disease.
“The mice have high blood sugar, high blood pressure. They have more lipids in the blood, and they also have more bone problems, as well,” Ramos said. “If you go to the clinic and ask a dentist to treat a patient with diabetes, they know that there will be some challenges. This is well-known, but why? Why do you have more failures in implants, for example, in a patient with diabetes? They will always be a periodontal patient because they have some underlying systemic condition. This is well-known that people with systemic disease, especially diabetes, obesity, dyslipidemia, hypertension, metabolic dysfunction in general, have poorer outcomes from therapeutic procedures.”
“So what we want with this study is to find causal links between these metabolic diseases and periodontal disease so that we can actually prevent this from happening,” Morandini said.
The duo doesn’t expect to have all of the answers after their five-year-long study, but they hope it will lay the foundation for catching periodontal disease early, creating improved treatments and prevention tactics for it and, in turn, metabolic diseases related to it. They hope this will be the groundwork for a scientific breakthrough that could change what we know about overall gum and metabolic health.
“We are building the foundation to say how the house can survive stress – the house is our body,” Morandini said. “So we need that foundation to know how the cells operate. What’s the mechanism inside the mitochondria that makes them communicate between tissues? If we can build knowledge of how to understand these mechanisms, then we can learn better strategies of how to prevent these diseases from happening.”
Uncovering more truths about periodontal disease to better serve the general public, putting taxpayer money to good use in creating a healthier world and training the future generation of researchers is what drives the couple to explore these medical pathways.
“It feels that we are on the right path – that we are moving the field forward by educating our students to be great health care providers and involving students in research so that they can be open-minded and think more critically to constantly evolve,” Morandini said.
Discoveries at Augusta University are changing and improving the lives of people in Georgia and beyond. Your partnership and support are invaluable as we work to expand our impact.
 Augusta University
Augusta University




