A portable ultrasound can help nephrologists better detect fluid in the lungs of patients with end-stage kidney disease, according to a study by physicians at the Medical College of Georgia at Augusta University.
Patients with the disease, characterized by the kidneys’ inability to work well enough to meet your body’s basic needs, can accumulate fluid all over their bodies, and commonly in the lungs says second-year nephrology fellow Dr. Omar Saleem.
The trick is knowing where the fluid is and how much needs to be removed, Saleem says, and accumulation in the lungs can lead to complications like heart failure and high blood pressure.
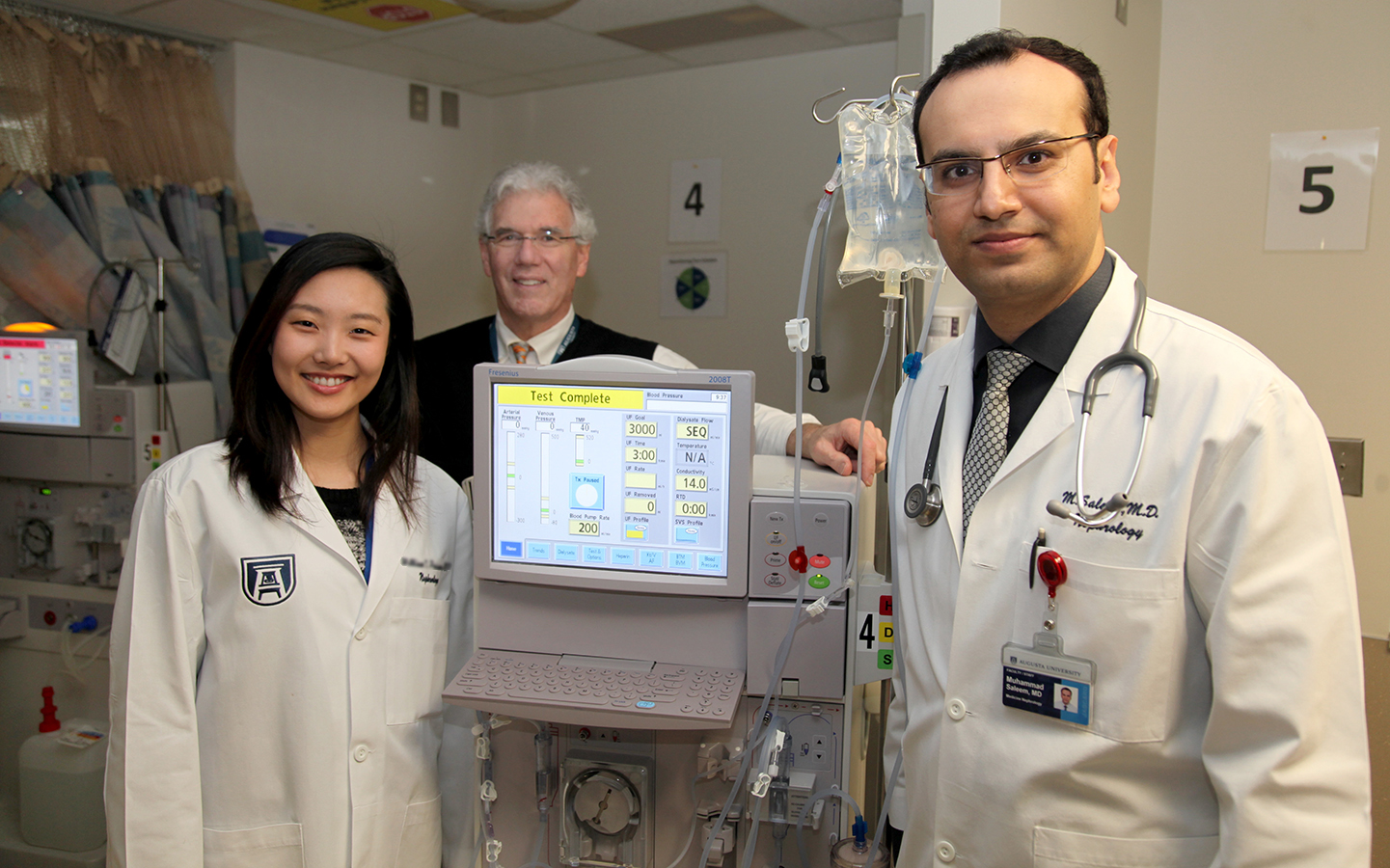
Saleem, and other faculty and students from MCG, will present their research at the Southern Regional Meetings of the American Federation for Medical Research this week in New Orleans.
When it comes to diagnosing “wet lungs,” the standard has been listening for chest crackling sounds with a stethoscope and measuring blood pressure – more fluid on the lungs prevents oxygen from being absorbed into the bloodstream. “But that’s quite subjective,” he says. “For instance, sometimes you can’t hear the crackling. That’s why the ultrasound adds to the physical exam.”
He examined 24 ESKD patients at Augusta University Health. As part of the normal physical exam, he placed the ultrasound probe on the patients’ chests to get a good view of the lungs. If there was fluid, he would see B-lines, which are actually reflections of the water in the lungs that appear as long, vertical white lines on an ultrasound. The higher the number of B-lines and the more intense, or bright, they were, the more fluid was present.
“This is an objective marker of lung water, the accumulation of which can lead to serious complications for already fragile patients. We’re right at the edge here and we’re trying to keep people from tipping over into heart failure,” says Dr. Stanley Nahman, MCG nephrologist and director of the Department of Medicine’s Translational Research Program. “This will change the way we manage these people with dialysis.”
Physicians can then better target dialysis treatments. “I can set the fluid removal goal at a higher point during dialysis,” Saleem says. “Where I might normally take off two liters of fluid, I might take three or four in someone who has water in their lungs”
“Our kidneys take all the fluid that comes from normal intake through diet and drinking and they filter the waste products, which we excrete in urine,” Nahman says “But these patients rarely urinate. They count on dialysis to keep their fluid in balance.” The kidneys also help the body reabsorb essential nutrients into the bloodstream.
Hemodialysis uses a special filter called a dialyzer – or an artificial kidney – to filter waste, balance electrolytes and remove extra fluid. End-stage kidney disease (ESKD) patients are typically receiving dialysis three times each week.
Also presenting is Dr. Elizabeth Chu, a second-year internal medicine resident and 2016 MCG graduate, who proposes a new way to manage the way former inmates with ESKD re-enter society.
The Georgia Department of Corrections is one of the largest state correctional systems in the country, supervising nearly 52,000 inmates – many of them have ESKD and are on three-times weekly dialysis at Augusta State Medical Prison. But there is currently no plan to help them figure out how to navigate treatment when they get out of prison, Chu says.
“We were finding that nephrologists were frequently called to the emergency room to provide dialysis to former inmates with ESKD and nowhere else to go,” she says. “When we consulted Augusta State Medical Prison regarding discharge of these patients, we found that most did not have active Medicare, which pays for dialysis. When they were released, inmates were given copies of their dialysis run sheets, documenting their treatments, the address of the nearest Social Security Office with instructions to ‘go sign up for Medicare’ and instructions to go to the ER for their dialysis until they got Medicare.”
With an average 12-week waiting period for Medicare, these former inmates were not eligible to enroll at private dialysis treatment centers, instead heading to their local emergency rooms for up to 36 treatments before they received insurance through Medicare.
“Not only was the funding gap resulting in erratic and inadequate care, but it also generated unnecessary costs borne by society,” Chu says.
A year of dialysis (150 treatments) in an outpatient facility costs about $89,000; one dialysis treatment in the Augusta University Medical Center Emergency Department is around $25,000. For a patient, receiving three treatments a week over 12 weeks costs could add up to around $900,000. The lack of regular medical care can also result in complications and unnecessary hospitalizations, which are also costly.
To define the scope of the problem, Chu reviewed the records of all ESKD patients at Augusta State Medical Prison from 2014-16, looking for demographic information and anticipated re-entry years. She also made comparisons to a national cohort.
Over the three-year study period, the prison had 180 dialysis patients. From this group, 73, or 41 percent, were discharged from the prison, which is an average of 24 patients per year – comparable to numbers for prison systems outside of Georgia.
“Assuming 24 re-entry patients per year at an ER dialysis cost of $900,000 per patient, the state could save around $21 million annually,” Chu said.
She proposes a Comprehensive Disease Management Program instead. Chu says hiring a re-entry navigator with a background in corrections social work and case management who initiates applications for Medicare four to six months before inmates are released would be a huge help. This navigator would also contact dialysis centers, hospitals and parole officers in the area where the inmate intended to live, and could have post-release visits at least monthly for two years, to make sure patients were following through with treatment plans.
Chu’s project was reviewed and endorsed by administrators of Augusta University, Georgia Correctional HealthCare, the Georgia Department of Corrections and the Office of the Governor. Georgia Correctional HealthCare is the division of Augusta University that provides high quality health care to over 60 Georgia Department of Correction facilities statewide.
Twelve other MCG students, residents and fellows are presenting their work at the meeting. Nahman and Dr. Stephanie Baer, chief of Infection Control and Epidemiology at the Charlie Norwood VA Medical Center, and Dr. Jennifer Waller, director of Clinical and Translational Science programs in the Department of Population Health Sciences, will also moderate a student panel on Big Data for the Clinician: An Approach to Data Mining Using the United States Renal Data System.
 Augusta University
Augusta University