Scientists are using “gene scissors” to cut off the code of a defective gene that results in progressively weaker muscles and death in Duchenne muscular dystrophy and replace it with a synthetic code they hope will one day restore healthy life to these patients.
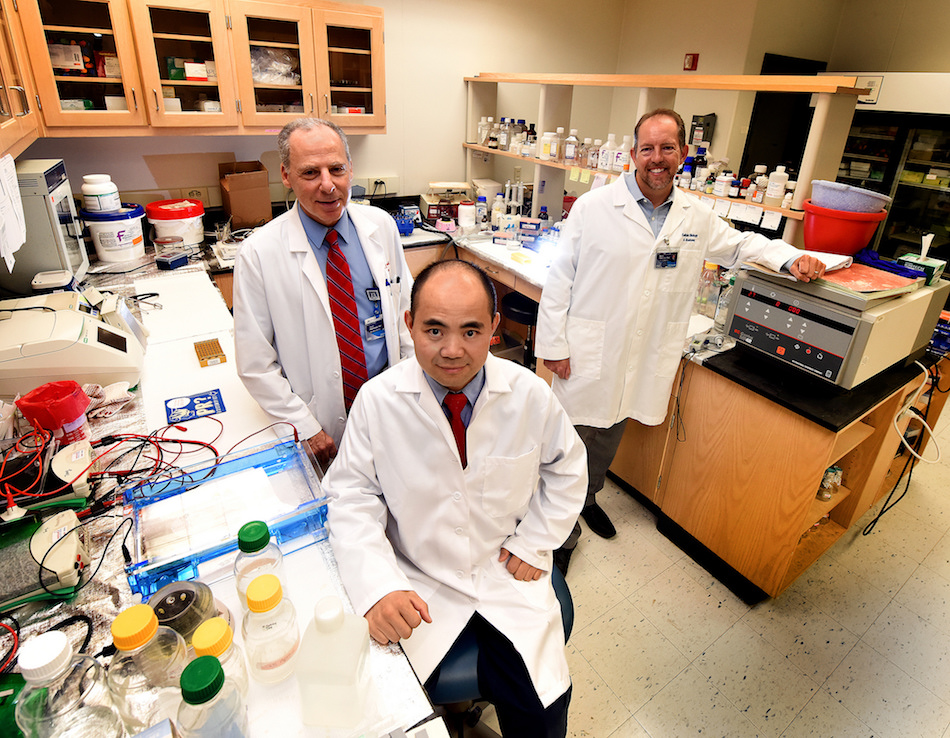
“We want to use genetically corrected stem cells to replace the stem cell pool and make new muscles that function normally,” said Dr. Yaoliang Tang, cardiovascular researcher in the Vascular Biology Center at the Medical College of Georgia at Augusta University. Tang is a principal investigator on a new $2.6 million National Institutes of Health grant that is enabling the studies in an animal model of the genetic disorder.
Every gene has a code that tells it what protein(s) it will ultimately express. In the case of the dystrophin gene in this disease, the code is telling the DNA to tell the RNA to make a short, dysfunctional form of dystrophin, a protein in the muscle cell membrane that is essential to the structural integrity of muscle cells.
“It’s a construction piece,” Dr. Mark Hamrick, bone biologist in the MCG Department of Cellular Biology and Anatomy, said of dystrophin.
Muscle cells are normally strong but constantly under stress as we move, breathe and exercise, often experiencing tears but typically rapid repair as well. But in these patients, muscle cells are weak, more prone to injury and death and end up being replaced with small, even weaker muscle fibers.
“You have so much regeneration that you get these weak little fibers; they are almost like a neonatal-type fiber; they are so small and weak,” Hamrick said. Healthy, strong muscle tissue is soon replaced by weak, dysfunctional fibrous tissue.
So the scientists are using technology called CRISPR-Cas9 to cut the problematic piece of the dystrophin gene out of muscle cells, and replace it with a synthetic code that enables normal dystrophin. They will ultimately return to their mouse model of Duchenne muscular dystrophy a progenitor muscle cell that is now expressing longer dystrophin and making stronger muscle cells that will eventually repopulate the weak muscle mass.
They are starting with muscle cells from the mouse model and reverting them to a stem-cell like state, called induced pluripotent stem cells. The pluripotent stem cells, which can make any cell type, can be derived from embryonic tissue, but a decade ago, Japanese scientists developed a method to make induced versions from essentially any cell type – such as a muscle cell – a development that would garner a Nobel Prize. The MCG scientists will coax the induced pluripotent stem cells to become muscle progenitor cells, the precursor for the healthy muscle cells needed.
The fact that the cells that will ultimately be returned, started with the individual – or the mouse in the case of this basic science study – also reduces concerns that giving the cells will result in a severe immune system response, Tang said. Gene editing also is more efficient in pluripotent stem cells than mature cells, he added.
The additional benefit of starting with a muscle cell is that cells have some genetic memory, so these have a predisposition to become muscle cells again, Tang said.
“It’s going to home to the muscle and differentiate into a muscle cell. So it’s going to go back in and rebuild everything,” said Hamrick, a co-investigator on the new grant.
One concern with using any type of stem cell is the possibility that these cells will also produce cancer. To diminish that possibility, Tang is adding a small molecule called Plurisin#1 to the mix that selectively targets stem cells for elimination. “After we do the gene editing and make the muscle progenitor cells, we just want to remove any tumor-potential pluripotent cells remaining before returning cells to the animal,” Tang said.
To further aid efficacy, they will use techniques like brief periods of ischemia and reperfusion in the muscles, a technique that Tang has shown will attract stem cells and enhance their activity. They also are engineering nano-sized compartments containing the stem-cell attracting protein SDF-1α for delivery to the dying muscle tissue.
CRISPR-Cas9 enables scientists to edit problematic genes by using the Cas9 enzyme for cutting and an RNA molecule that helps identify the right target. The technology can be used to edit a gene, and, as in the case of Tang’s study, to also reinsert a substitute.
Duchenne muscular dystrophy is one of nine types of muscular dystrophy, according to the Muscular Dystrophy Association. Symptoms of weakness tend to rise between the ages of 3-5 in the condition that is far more common in males. Early on, patients can have trouble standing, keeping their balance and raising their arms. Death often results from respiratory and/or heart failure, since strong muscles are needed to drive these basic life functions.
This fall, scientists at China’s Sichuan University became the first to use the technology clinically to disable a gene, which can block the immune response, in the immune cells of a patient with aggressive lung cancer. Cancer typically uses the gene to its advantage to weaken the body’s attack against it. The scientists then increased the immune cell number and injected them back into the patient. Additional trials are expected next year.
It likely will be several years before the MCG scientists know whether their basic science studies will result in these types of clinical trials for patients with Duchenne muscular dystrophy, Tang and Hamrick said.
Current therapies for Duchenne muscular dystrophy include steroids, bracing and physical therapy. Earlier this year, the Food and Drug Administration approved the drug eteplirsen for patients, a controversial decision – despite the welcome news for parents and children – because the clinical trial was only in a dozen patients and because of questions about whether the drug sufficiently increases levels of dystrophin.
Dr. Neal L. Weintraub, associate director of MCG’s Vascular Biology Center and Georgia Research Alliance Herbert S. Kupperman Eminent Scholar in Cardiovascular Medicine, also is a principal investigator on the multiple principal investigator NIH grant.
 Augusta University
Augusta University