Whether ablation of the highest-risk heart arrhythmia is best handled by a robot or the hands of an electrophysiologist should be answered by an international comparison of the two.
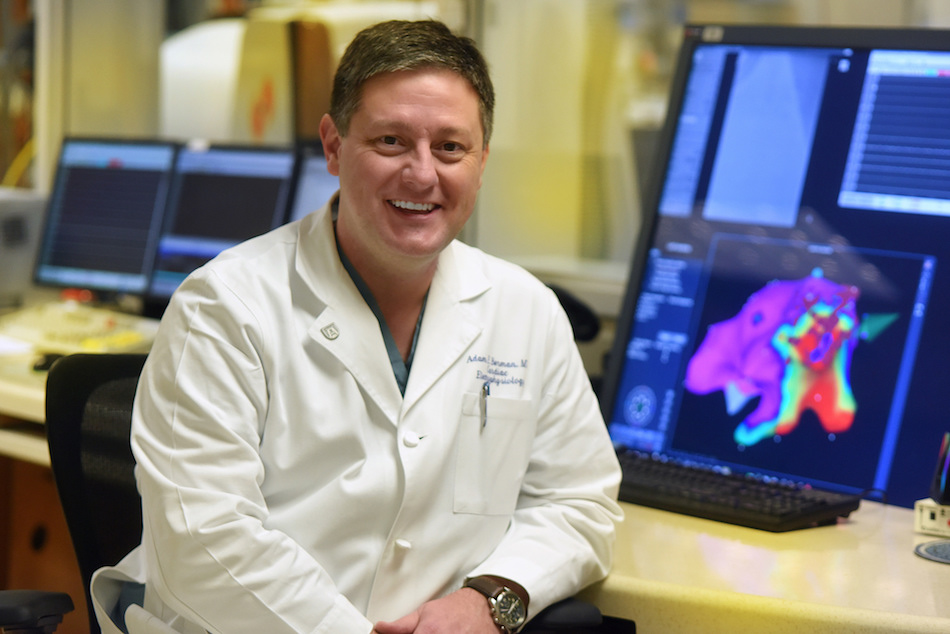
These are high-risk scenarios where physicians first identity the area of a beating heart that is the source of the rapid, potentially deadly ventricular tachycardia, then destroy it, said Dr. Adam E. Berman, associate professor of medicine and pediatrics at the Medical College of Georgia at Augusta University and director of Cardiac Arrhythmia Ablations Services at AU Medical Center.
“You want your energy delivery to be as appropriate and precise as possible,” said Berman, a principal investigator on the side-by-side comparison of the two approaches in nearly 400 patients with ventricular tachycardia at more than a dozen centers, including AU Medical Center. The study is funded by Stereotaxis, which manufactures the Niobe ES remote magnetic navigation system used at AU Medical Center and others.
The robotic system has GPS to help ensure the most direct path to the problematic heart area. While it does not reduce invasiveness in cardiac ablation, as it does in procedures such as a hysterectomy, it does quite literally enable even subfractional movement – down to one millimeter or 0.039 inches – of the flexible catheter to further maximize accuracy. The robotic arm also can stay where needed indefinitely, said Berman, “whereas I could wear out.”
Manual ablation – which remains the standard approach in this country – has the electrophysiologist at the bedside maneuvering a more-rigid, heat-producing catheter to the focal point of the abnormal electrical signals and holding it there until ablation is complete. Procedures can take about two hours.
“You begin to accept that partnering with a machine can potentially deliver way better outcomes than doing it without it,” said Berman. It also could open the door to the electrophysiologist being at one location and the patient at another.
Berman’s experience with robotics has shown that for many arrhythmias, including the common and chaotic atrial fibrillation, his hands are typically better and/or faster. But for ventricular tachycardia, he almost always opts for the remote navigation system, unless, for example, the patient’s anatomy precludes it. Still he welcomes the opportunity to find out if robotics holds up as the best option in a broader comparison of outcomes. “We need to know,” Berman said.
The study is in adults with ischemic ventricular tachycardia, the most common type of this increasingly common arrhythmia. Enrollees must also have an implantable defibrillator and drug-resistant arrhythmia. Key exclusionary factors include a heart attack within the past 30 days, cardiac surgery within the past 60 days, unstable chest pain and previous ablation. Patients are being followed for a year for recurrence of ventricular tachycardia. Researchers also will be assessing how often the defibrillator had to shock a patient, how long the procedure took and more.
Ventricular tachycardia is so common post-heart attack that many patients get an implantable defibrillator that can shock the heart back into normal rhythm, at least temporarily, if the rapid rhythm occurs. The fact that more people are surviving heart attacks means the incidence of the potentially deadly arrhythmia likely will only continue to increase, Berman said. Defibrillators have enabled patients to live with the condition, but particularly when episodes become more frequent, patients may start looking for other options because of concerns such as being shocked repeatedly, potentially feeling faint and unable to drive, and more, Berman said. Ablation, alternatively, can eliminate ventricular tachycardia by modifying the scar tissue generating it.
Ventricular tachycardia starts in either of the pumping chambers of the heart where most heart attacks occur, Berman said. Even years afterward, scar tissue resulting from heart attack can begin to generate rapid abnormal rhythms that can interfere with the heart pumping blood, causing fainting and sudden cardiac arrest.
The heart’s natural pacemaker sets the heart rate based on demand, whether you are sitting on the couch or walking on the treadmill. “It sends out little electrical tweets that tell your heart to beat. Every time it does that, all the heart muscle is supposed to react in a certain way.” Berman said. “But scar tissue does not conduct electricity in the proper way. Scar tissue sets the stage for having arrhythmias.”
Georgia has two of the remote magnetic navigation systems and many surrounding states have none. AU Medical Center and Berman get referrals for patients with ventricular tachycardia from across the southeastern United States. “Centers with magnetic navigation technology tend to attract referrals for ablation of ventricular tachycardia,” Berman said.
Last year, the robotic system was used in about 2,300 of the 60,000 ventricular tachycardia ablations performed worldwide, according to Stereotaxis. Treatment with the system typically is more costly than the manual approach.
For more information, contact Berman at 706-721-4997.
 Augusta University
Augusta University